Spread To The Western Hemisphere
Further isolated occurrences of this infection may have been emerging as early as 1966. The virus eventually entered gay male communities in large United States cities, where a combination of casual, multi-partner sexual activity and relatively high transmission rates associated with anal intercourse allowed it to spread explosively enough to finally be noticed.
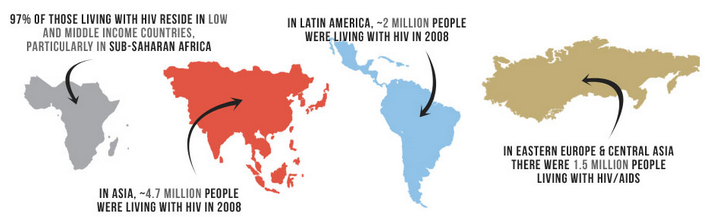
Because of the long incubation period of HIV before symptoms of AIDS appear, and because of the initially low incidence, HIV was not noticed at first. By the time the first reported cases of AIDS were found in large United States cities, the prevalence of HIV infection in some communities had passed 5%. Worldwide, HIV infection has spread from urban to rural areas, and has appeared in regions such as China and India.
Origin And Epidemic Emergence
Several of the theories of HIV origin accept the established knowledge of the HIV/SIV phylogenetic relationships, and also accept that bushmeat practice was the most likely cause of the initial transfer to humans. All of them propose that the simultaneous epidemic emergences of four HIV groups in the late 19th-early 20th century, and the lack of previous known emergences, are explained by new factor that appeared in the relevant African regions in that timeframe. These new factor would have acted either to increase human exposures to SIV, to help it to adapt to the human organism by mutation , or to cause an initial burst of transmissions crossing an epidemiological threshold, and therefore increasing the probability of continued spread.
Genetic studies of the virus suggested in 2008 that the most recent common ancestor of the HIV-1 M group dates back to the Belgian Congo city of Léopoldville , circa 1910. Proponents of this dating link the HIV epidemic with the emergence of colonialism and growth of large colonial African cities, leading to social changes, including a higher degree of non-monogamous sexual activity, the spread of prostitution, and the concomitant high frequency of genital ulcer diseases in nascent colonial cities.
Social changes and urbanization
Colonialism in Africa
This theory was later dubbed “Heart of Darkness” by Jim Moore, alluding to the book of the same title written by Joseph Conrad, the main focus of which is colonial abuses in equatorial Africa.
The Patient Zero Myth
For decades, a French-Canadian airline employee named Gaetan Dugas, has been known as Patient Zero in the 1980s AIDS epidemic.
Dugas, a man who had sex with men , died in 1984. Since then he has been blamed by some as a primary source for the spread of HIV in North America.
Dugas was one of the primary villains in the 1987 book, And the Band Played On, by San Francisco journalist Randy Shilts.
However, the researchers now say Dugas was falsely accused and unfairly blamed.
Gaetan Dugas is one of the most demonized patients in history, and one of a long line of individuals and groups vilified in the belief that they somehow fueled epidemics with malicious intent, said Richard McKay, D.Phil., a Wellcome Trust Research Fellow in Cambridges Department of History and Philosophy of Science, in a press release.
In fact, McKay says, Dugas actually provided scientists with valuable information before he died.
Dugas told researchers after he contracted HIV that he had 750 sexual partners the previous three years. That wasnt necessarily an unusual number. Researchers said 65 percent of men in a Los Angeles cluster study at the time reported having more than 1,000 sexual partners in their lifetimes.
Much of that sexual connection was with anonymous partners, so many HIV patients couldnt give medical officials any names.
However, McKay says, Dugas provided medical officials with 72 names. That helped scientists track down a wide range of people infected with HIV.
You May Like: What Happens When Hiv Enters The Body
How Are Siv And Hiv Related
According to research, HIV is directly linked to SIV. There are various similarities between the two viruses. HIV-1, in particular, is closely related to a strain of SIV, which can be found in chimpanzees. HIV-2, on the other hand, is linked with a strain of SIV found in sooty mangabeys.
The Simian Immunodeficiency Virus attacks the immune systems of monkeys and apes. The Human Immunodeficiency Virus follows a similar pattern of infection. It is a type of lentivirus that targets the human immune system.
The Blood Bank Community’s Statement
A week after the Atlanta meeting in January 1983, the American Association of Banks, the Council of Community Blood Centers, and the American Red Cross issued a joint statement that ”direct or indirect questions about a donor’s sexual preference are inappropriate.” The statement recommended questions to detect possible exposure , but did not recommend any laboratory screening tests. At this time, the PHS agencies had not completed their own recommendations , and the FDA did not issue any recommendations.
You May Like: Do You Need To Fast For Hiv Blood Test
Years Of Aids: A Timeline Of The Epidemic
Over the past four decades, UCSF has led the way in its heroic and committed response to the AIDS epidemic, both locally and globally. This timeline covers some of the highlights over the past 40 years at UCSF, in the nation and around the world after a mysterious outbreak affecting gay men was first reported on June 5, 1981.
Why Do We Care Does All This Research Into How The Virus Got Started Tell Us Anything About How To Stop It
Hunting chimps in West Central Africa.
Research into the HIV’s origins may eventually yield practical results. It could help scientists understand why HIV’s viral ancestor, SIV, doesn’t kill or even sicken chimps who carry it. With that knowledge, researchers might be able to make drugs with fewer side effects, or broad-spectrum vaccines that protect against all the strains of the disease that infect people today.
Korber suggests that in an era of emerging diseases, looking back on the virus’ shadowy origins offers a “history lesson,” or perhaps even a fable, with a moral attached. By the time doctors realized that HIV/AIDS existed, it had already taken up permanent residence in humans. They couldn’t have known about it before then, but, Korber says, at least now they know to be wary as the virus continues its shape-shifting spread around the globe. “The fact that it could be with us for quite a long time before we even realized it was there is kind of eye-opening,” she says. “I think it’s something to keep us on our toes. It helps us understand that we can be surprised.” And of course, HIV research may have a few surprises left for us, too.
Recommended Reading: What Is Used To Treat Hiv Aids
Position Of The National Hemophilia Foundation
The next day, the Medical and Scientific Advisory Council of the NHF met and recommended that cryoprecipitate , rather than AHF concentrate, be used for newborn infants and children under four, newly diagnosed patients, and those with mild hemophilia. According to the report, there was insufficient evidence to develop specific recommendations about blood product use in the treatment of severe hemophilia. Additional recommendations included delaying all elective surgical procedures and the use of a synthetic substance, DDAVP , to elevate Factor VIII levels in patients with mild or moderate hemophilia A. MASAC also stated that it was important to screen and exclude all high-risk donors from the blood and plasma supply for the production of blood products used for treatment of hemophilia. The NHF directed their recommendations to treating physicians, regional and community blood collection centers, and plasma fractionators in some instances, the NHF also told their chapters to distribute the information to the chapter members.
Why Do Scientists Look At Recent Samples Of Hiv To Determine The Virus’ Overall Age Wouldn’t It Be Better To Use Older Samples That Haven’t Had As Much Time To Mutate
It would, but scientists don’t have that luxury. Other than the 1959 sample, there are very few preserved specimens of HIV-infected tissue that predate the early ’80s, when the virus was first recognized by health authorities. Researchers still hope there are forgotten samples in African freezers. “There has to be some serum or plasma somewhere, and given modern technology we could fish out the virus,” says Dr. David Ho, director of the Aaron Diamond AIDS Research Center and one of the world’s leading authorities on HIV.
But even if those samples are found someday, they won’t necessarily yield definite answers about the virus’ age, says Korber: “Often, you can’t get anything out of samples like that.” Most African samples are made of blood serum, and serum samples contain viral RNA, which degrades much faster than the DNA found in tissue samples. In fact, says Ho, the 1959 sample, which was sequenced by his laboratory, was kept in a freezer but still didn’t survive the ravages of time. “It was completely dried up,” he says. “We were only able to get small pieces , and we had to stitch them together.”
Don’t Miss: Can Hiv Be Tested At Home
Are There Other Theories About How The Virus Could Have Gotten Into Humans
There are several competing theories, ranging from implausible conspiracies to arguments grounded in extensive research. The best-known of the latter, the “OPV/AIDS” theory, was exhaustively detailed in the 1999 book The River, by author Edward Hooper. As many as a million Africans were given oral polio vaccines between 1957 and 1960. Hooper says witnesses have told him that a few batches of those vaccines were “grown” in chimp cells at a lab in Kisangani, a city in the Democratic Republic of the Congo — and that the chimp cells, and thus the vaccines, could have contained SIVs that jumped into humans. “There are highly significant correlations between the places where this vaccine was administered and the places where ⦠AIDS first appeared on the planet four to 20 years later,” Hooper says.
The majority of HIV researchers subscribe to the bushmeat theory and raise several arguments against the OPV theory. Hahn’s recent research confirming that HIV-1 M and N arose from Pan troglodytes troglodytes chimps in Cameroon presents one problem: The Kisangani lab is in the Democratic Republic of the Congo, and it’s home to a different subspecies of chimp than the one that was the source of HIV-1 M and N. However, it is possible that the chimps used in the Kisangani experiments were not from the area. In the spring of 2006, Hooper found a paper indicating that at least one of eight chimps at the Kisangani lab was a Pan troglodytes troglodytes.
Position Of The Plasma Fractionation Industry
On January 28, 1983, the American Resources Association , which represents the plasma industry, issued recommendations about donor screening and deferral to reduce the risk of . The recommendations focused on donor education, donor screening, and surrogate laboratory testing. The ABRA recommended issuing a brochure that would describe AIDS, tell how individuals in high-risk groups could reduce their risk of exposure, and discourage high-risk persons from donating. The ABRA also recommended that prospective donors, prior to donating, be required to read the information about AIDS and indicate that they were not members of a high-risk group. Individuals who identified themselves as members of high-risk groups or were unwilling to reply would be excluded from donating plasma . The ABRA recommended against large-scale surrogate testing of donated blood until ABRA had evaluated its feasibility.
Read Also: Can You Donate Plasma With Hiv
A Vivid 1983 Reminder Of Initial Aids Scare
Even as the nation’s attention was directed toward gay AIDS victims, the virus was replicating in the bloodstreams of hemophiliacs and injection drug users. A government report from August 2016 found that between the start of the AIDS epidemic and today, nearly 700,000 people have died of AIDS in the U.S.
Activism By Aids Patients And Families

In New York City, Nathan Fain, Larry Kramer, Larry Mass, Paul Popham, Paul Rapoport, and Edmund White officially established the Gay Men’s Health Crisis in 1982.
Also in 1982, Michael Callen and Richard Berkowitz published How to Have Sex in an Epidemic: One Approach. In this short work, they described ways gay men could be sexual and affectionate while dramatically reducing the risk of contracting or spreading HIV. Both authors were themselves gay men living with AIDS. This booklet was one of the first times men were advised to use condoms when having sexual relations with other men.
At the beginning of the AIDS epidemic in the 1980s, there was very little information about the disease. Also, because AIDS affected stigmatized groups, such as LGBTQ and people of low socioeconomic status, there wasn’t much mass media coverage initially when the epidemic started. However, with the rise of activist groups composed of people suffering from AIDS, either directly or through a loved one, more public attention was brought to the epidemic.
Don’t Miss: Which Cells Does Hiv Attack
New Cdc Director Predicts Us Can End Aids Epidemic Within Seven Years
Accumulated data from several studies show that in nearly 80,000 condomless sex acts between pairs of men who had discordant HIV status one was negative, the other was positive, but virally suppressed not a single new infection occurred.
In the HIV world, that finding has given rise to a slogan: U = U, or undetectable equals untransmissible. To maximize the benefits of viral suppression, though, people must know their HIV status and start treatment if they are infected. Currently the CDC estimates that 15 percent of infected Americans are unaware they are HIV positive.
People with HIV infection need to be diagnosed, getting care, stay in care, get on antiretrovirals, and get their viral load down to undetectable, Redfield said.
Pairing the power of viral suppression with another tool further increases the chances of stopping spread of the virus. That other tool is PrEP, pre-exposure prophylaxis antiretroviral drugs used to prevent infection in people who are at high risk of contracting the virus.
Taken correctly, PrEP reduces the risk of contracting HIV from an infected partner by 95 percent. If the infected partner is virally suppressed, the risk is lower still.
Paradoxically, doctors bear part of the blame for that gap.
In some cases, the problem of too little PrEP prescribing is due to a lack of training, and in other cases, something else may be at play, suggested Dr. Demetre Daskalakis, the New York Department of Healths deputy commissioner of disease control.
Unresolved Questions About Hiv Origins And Emergence
The discovery of the main HIV / SIV phylogenetic relationships permits explaining broad HIV biogeography: the early centres of the HIV-1 groups were in Central Africa, where the primate reservoirs of the related SIVcpz and SIVgor viruses exist similarly, the HIV-2 groups had their centres in West Africa, where sooty mangabeys, which harbour the related SIVsmm virus, exist. However, these relationships do not explain more detailed patterns of biogeography, such as why epidemic HIV-2 groups only evolved in the Ivory Coast, which is one of only six countries harbouring the sooty mangabey. It is also unclear why the SIVcpz endemic in the chimpanzee subspecies Pan troglodytes schweinfurthii did not spawn an epidemic HIV-1 strain to humans, while the Democratic Republic of Congo was the main centre of HIV-1 group M, a virus descended from SIVcpz strains of a subspecies that does not exist in this country. It is clear that the several HIV-1 and HIV-2 strains descend from SIVcpz, SIVgor, and SIVsmm viruses, and that bushmeat practice provides the most plausible cause of cross-species transfer to humans. However, some loose ends remain.
It is not yet explained why only four HIV groups spread considerably in human populations, despite bushmeat practices being widespread in Central and West Africa, and the resulting human SIV infections being common.
Also Check: What Is The Hiv Aids Rate In The United States
The Public Health Service Effort
As discussed earlier, the PHS Committee on Opportunistic Infections in Patients with held its second meeting on July 27, 1982. On the same date, the committee distributed two recommendations to the assistant secretary for health, the FDA commissioner, the NIH director, CDC regional offices, and state and territorial health officers. The first recommendation was to establish an active surveillance system at once to identify new suspected cases of occurring in individuals with hemophilia. In November, the CDC, the NHF, and the regionally based network of hemophilia treatment centers agreed to cooperate in this effort. The second recommendation called for laboratory studies of the immunologic competence of individuals with hemophilia who had no symptoms of opportunistic infections, and applied research to determine practical techniques for eliminating the risk of infection from AHF concentrate . The meeting summary also noted concerns about the adequacy of funding to support these activities, stating that existing federal grants and contract mechanisms were not “responsive to rapid funding of urgent problems” .
New Study Shows Hiv Epidemic Started Spreading In New York In 1970
A new genetic study confirms theories that the global epidemic of HIV and AIDS started in New York around 1970, and it also clears the name of a gay flight attendant long vilified as being “Patient Zero.”
Researchers got hold of frozen samples of blood taken from patients years before the human immunodeficiency virus that causes AIDS was ever recognized, and teased out genetic material from the virus from that blood.
They use it to show that HIV was circulating widely during the 1970s, and certainly before people began noticing a gay plague in New York in the early 1980s.
Also Check: When Do You Get Hiv Symptoms
Reconsidering The Evidence: Further Attempts To Formulate Policies
In the interval between the decisions of early 1983 and discovery of the virus that causes in early 1984, public health and blood industry officials became more certain that AIDS was a blood-borne disease as the number of reported cases of AIDS among hemophiliacs and transfused patients increased. As their knowledge grew, these officials had to decide about recall of contaminated blood products and possible implementation of a surrogate test for HIV. Major opportunities to reconsider the policies of early 1983 arose at meetings of the FDA’s Product Advisory Committee in July and December 1983.
On May 11, 1983, Hyland Therapeutics recalled a lot of AHF concentrate when it discovered that the product had been manufactured from pools containing plasma from an individual subsequently diagnosed as having . The NHF issued a medical bulletin and a chapter advisory in conjunction with the recall, stating:
It is not the role of the NHF to judge the appropriateness of corporate decisions made by individual pharmaceutical companies. However, we urge that patients and treaters recognize the need for careful evaluation of blood products and note that such a recall action should not cause anxiety or changes in treatment programs. The NHF recommends that patients maintain the use of concentrates or cryoprecipitate as prescribed by their physicians. If you have any questions regarding this matter, they should be directed to your treating physician and/or the NHF .