Transmission Of Hiv Infection
The transmission of HIV requires contact with a body fluid that contains the virus or cells infected with the virus. HIV can appear in nearly any body fluid, but transmission occurs mainly through blood, semen, vaginal fluids, and breast milk. Although tears, urine, and saliva may contain low concentrations of HIV, transmission through these fluids is extremely rare, if it occurs at all.
HIV is not transmitted by casual contact or by close, nonsexual contact at work, school, or home. No case of HIV transmission has been traced to the coughing or sneezing of an infected person or to a mosquito bite. Transmission from an infected doctor or dentist to a patient is extremely rare.
HIV is usually transmitted in the following ways:
HIV is more likely to be transmitted if skin or a mucous membrane is torn or damagedeven if minimally.
In the United States, Europe, and Australia, HIV has been transmitted mainly through men who have sex with men and the sharing of needles among people who inject drugs, but transmission through heterosexual contact accounts for about one fourth of cases. HIV transmission in Africa, the Caribbean, and Asia occurs primarily between heterosexuals, and HIV infection occurs equally among men and women. In the United States, fewer than 25% of adults who have HIV infection are women. Before 1992, most American women with HIV were infected by injecting drugs with contaminated needles, but now most are infected through heterosexual contact.
Interval Of Mild Or No Symptoms
After the first symptoms disappear, most people, even without treatment, have no symptoms or only occasionally have a few mild symptoms. This interval of few or no symptoms may last from 2 to 15 years. The symptoms that most commonly occur during this interval include the following:
-
Swollen lymph nodes, felt as small, painless lumps in the neck, under the arms, or in the groin
-
White patches in the mouth due to candidiasis
-
Anemia
Some people progressively lose weight and have a mild fever or diarrhea.
These symptoms may result from HIV infection or from opportunistic infections that develop because HIV has weakened the immune system.
Why Does The Immune System Fail To Fight The Hiv Virus
There are various reasons which can contribute to the failure of the immune system to control HIV infection and prevent AIDS development. By infecting CD4+ T cells, HIV is able to replicate predominantly in activated T cells and paralyse one of the main components of adaptive immune system. HIV can also establish latent infection in CD4+ T cells and remain invisible to CD8+ T cells and therefore replication can occur later in the infection and generate new virions. Antigenic mutation within the T-cell epitopes can affect the binding capacity of MHC molecules to the viral peptides, resulting in the inability of the TCRs to recognise the MHC-peptide complex. Finally, HIV is able to hide from anti-HIV antibodies by expressing non-immunogenic glycans on key antibody epitopes.
Also Check: Hiv Stays Alive In Dried Blood
Homeostasis Of Memory Cd4+ T Cells In Health
The CD4+ T cell pool comprises naive cells and heterogeneous memory populations. The mechanisms by which memory cells are maintained are not completely defined , but survival and self-renewing proliferation are likely to be controlled by competition for homeostatic resources such as cytokines and TCR-self-peptide/MHC interactions, and rates of turnover may vary between memory subpopulations . In uninfected individuals, depletion of CD4+ T cells results in compensatory homeostatic proliferation . This observation has led to the concept of T cell niches, either at the level of the memory cell compartment as a whole , or at the level of individual clones .
With HIV infection in mind, and building on earlier studies , we propose a model of healthy memory CD4+ T cell homeostasis that distinguishes between resting cells and cells that have received homeostatic division signals and so are transiently activated .
How Does Hiv Transmit In The Body
This is the basic pathway of HIV. The virus can get inside the body through our bodily fluids, particularly blood, semen for men, vaginal fluid for women, and even breast milk from infected mothers.
Since the virus targets the bodys immune system, its first victim or host cell would be the T-helper cells . It attaches and invades these white blood cells and takes control of the cell overall. Once the virus manages to infiltrate the DNA of the CD4 cells, it can now replicate and make copies of the infected CD4 cells, spreading it all over the body via your bloodstream.
The CD4 cells are then destroyed, and the HIV that rides on the host cell then takes over the duplication and spread of the virus. If left untreated, your CD4 cell count goes down to severely low levels, indicating the advancement of your HIV infection to AIDS.
One can categorize HIV infection into 3 acute, chronic, and the advanced stage called AIDS.
Read Also: How Long From Hiv To Aids
No Longer A Death Sentence: How Living With Hiv Has Changed
HIV has proved extraordinarily difficult to eradicate from the body because it will infect certain long-lived immune cells, known collectively as the viral reservoir, that can spend lengthy periods in a resting state. This keeps the viral DNA, known as provirus, that is encoded into those cells under the radar of standard antiretroviral treatment, which can only attack the virus in infected cells when they are actively churning out new copies of HIV.
Yu was also the lead author of a paper in Nature in August 2020 that analyzed 64 people who, like the Argentine woman, are so-called elite controllers of HIV. These are among the estimated 1 in 200 people with HIV whose own immune systems are somehow able to suppress the viruss replication to very low levels without antiretrovirals.
That studys authors found that these individuals immune systems appeared to have preferentially destroyed cells that harbored HIV capable of producing viable new copies of the virus. Left over were only infected cells in which the viral genetic code was spliced into a kind of genetic dead zone regions of the cellular DNA that were too distant from the levers that propel viral replication.
One member of that cohort, Loreen Willenberg, a now-67-year-old Californian who was diagnosed with HIV in 1992, stood out as having an immune system that had apparently vanquished the virus entirely. Even after sequencing billions of her cells, scientists could not find any intact viral sequences.
Adaptive Immune Response To Hiv
Cellular immune response to HIV. The cellular immune response is induced upon the entry of HIV into the target cells and synthesis of viral proteins . MHC class I on the cell surface displays the intracellularly degraded HIV peptide fragments for recognition by T-cell receptors on CD8+ T cells . CD8+ T cells lyse HIV infected cells and secrete cytokines, i.e. interferon- , tumor necrosis factor , and chemokines, i.e. MIP-1 , MIP and RANTES, that inhibit virus replication and block viral entry into CD4+ T cells. Development of CD8+ T cells is crucial for control of HIV replication. This results in declining viraemia after primary infection. In the early stages of infection, CD4+ T cells lose their proliferative capacity and therefore their contribution to viral control is minor. However, during chronic infection CD4+T cells are present and secrete interleukin-2 or cytokines, such as IFN-, to control viraemia.
Figure 3.
Don’t Miss: Can You Get Aids From Dried Blood
The Intersection Of Viral Fitness And Immune Control
Although most of the focus on immune control and lack of control has been on CD8+ T-cell function and differential induction of negative immunoregulatory molecules, an increasing body of data suggests that immune-mediated mutations within CD8+ T-cell epitopes lead to reduced viral fitness. These data include assays in which replication of virus containing a B57-selected mutation is out-competed by wild-type virus , evidence of reduced viral fitness in Gag-PR in persons who control virus spontaneously , and evidence of compensatory mutations leading to restoration of fitness . Importantly, mutations in Env do not lead to reduced fitness, suggesting that structural constraints are likely key to this effect . More recent studies have shed further light on this, by demonstrating that there are multidimensional constraints on HIV evolution because certain combinations of mutations must occur in a coordinated manner to maintain virus viability, and thus constrain immune escape pathways . Persons who spontaneously control HIV without medications preferentially target sites that are most constrained, providing further evidence that the specific sites targeted by the immune system may have a major impact on overall control .
Contributors To Cd4+ T
CD4+ T-cells are known to be the central facilitators for both cellular and humoral immune responses against exogenous antigens and are kept constant in the human body by homeostatic mechanisms .HIV binds to the CD4 molecule on the surface of helper T-cells and replicates within them. This results in destruction of CD4+ T-cells and leads to a steady decline in this population of T-cells. The definition of progressive and slow loss of CD4+ T-cells is not clear. In order to understand the correlation between CD4+ T-cell depletion and immunopathogenesis, and its relationship with disease progression, a number of dynamic models have been put forward. Two of the most acknowledged mechanisms are discussed in detail in this review. These include direct virus attack leading to cytolytic effect and chronic immune activation resulting in apoptosis.
Recommended Reading: Do Youngboy Got Herpes
What Do These Findings Mean
These results show that a slow process must be active in the HIV-induced depletion of CD4+ cells. Because of its simplicity, the model used in this study is convincing in its rejection of the runaway hypothesis, but a more detailed analysis will be needed to tell us precisely what the slow process is. One possibility raised by the authors is that this process is the slow adaptation of the virus itself over the course of infection. Specifically identifying this process will provide a key insight into the nature of HIV disease and indicate potential new approaches to therapy.
Preventing Transmission From Mother To Newborn
Pregnant women infected with HIV can transmit the virus to the newborn.
The following can help prevent HIV transmission from mother to newborn Prevention of transmission for infected mothers Human immunodeficiency virus infection is a viral infection that progressively destroys certain white blood cells and causes acquired immunodeficiency syndrome . Human immunodeficiency… read more :
-
Testing pregnant women to determine whether they are infected with HIV
-
If they are infected, treating them with antiretroviral drugs during pregnancy and labor
-
Delivering the baby by cesarean rather than by vaginal delivery
-
After birth, treating the newborn with zidovudine, given intravenously, for 6 weeks
-
If possible, using formula instead of breastfeeding
Don’t Miss: Can Hiv Cause Hair Loss
How Does Acute Hiv Affect The Body
Once a person contracts HIV, the acute infection takes place immediately.
Symptoms of the acute infection may take place days to weeks after the virus has been contracted. During this time, the virus is multiplying rapidly in the body, unchecked.
This initial HIV stage can result in flu-like symptoms. Examples of these symptoms include:
- myalgias, or muscle pain
However, not all people with HIV experience initial flu-like symptoms.
The flu symptoms are due to the increase of copies of HIV and widespread infection in the body. During this time, the amount of CD4 cells starts to fall very quickly. The immune system then kicks in, causing CD4 levels to rise once again. However, the CD4 levels may not return to their pre-HIV height.
In addition to potentially causing symptoms, the acute stage is when people with HIV have the greatest chance of transmitting the virus to others. This is because HIV levels are very high at this time. The acute stage typically lasts between several weeks and months.
How Does Chronic Hiv Affect The Body
The chronic HIV stage is known as the latent or asymptomatic stage. During this stage, a person usually wont have as many symptoms as they did during the acute phase. This is because the virus doesnt multiply as quickly.
However, a person can still transmit HIV if the virus is left untreated and they continue to have a detectable viral load. Without treatment, the chronic HIV stage can last for many years before advancing to AIDS.
Advances in antiretroviral treatments have significantly improved the outlook for people living with HIV. With proper treatment, many people who are HIV-positive are able to achieve viral suppression and live long, healthy lives. Learn more about HIV and life expectancy.
A normal CD4 count ranges from approximately 500 to 1,600 cells per cubic millimeter of blood in healthy adults, according to HIV.gov.
A person receives an AIDS diagnosis when they have a CD4 count of fewer than 200 cells/mm3.
A person may also receive an AIDS diagnosis if theyve had an opportunistic infection or another AIDS-defining condition.
People with AIDS are vulnerable to opportunistic infections and common infections that may include tuberculosis, toxoplasmosis, and pneumonia.
People with weakened immune systems are also more susceptible to certain types of cancer, such as lymphoma and cervical cancer.
The survival rate for people with AIDS varies depending on treatment and other factors.
You May Like: How Long Does It Take To Become Undetectable Hiv
Through Blood Transfusions Or Organ Transplants
Currently, HIV infection is rarely transmitted through blood transfusions or organ transplants.
Since 1985 in most developed countries, all blood collected for transfusion is tested for HIV, and when possible, some blood products are treated with heat to eliminate the risk of HIV infection. The current risk of HIV infection from a single blood transfusion is estimated to be less than 1 in about 2 million in the United States. However, in many developing countries, blood and blood products are not screened for HIV or are not screened as stringently. There, the risk remains substantial.
HIV has been transmitted when organs from infected donors were unknowingly used as transplants. HIV transmission is unlikely to occur when corneas or certain specially treated tissues are transplanted.
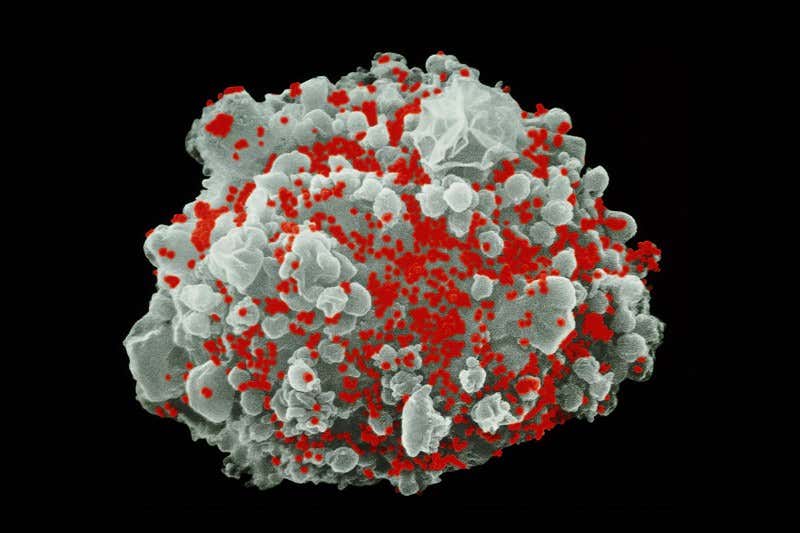
Mechanism Of Hiv Infection
Once in the body, HIV attaches to several types of white blood cells. The most important are certain helper T lymphocytes involves white blood cells that travel through the bloodstream and into tissues, searching for and attacking microorganisms and… read more ). Helper T lymphocytes activate and coordinate other cells of the immune system. On their surface, these lymphocytes have a receptor called CD4, which enables HIV to attach to them. Thus, these helper lymphocytes are designated as CD4+.
). Once inside a CD4+ lymphocyte, the virus uses an enzyme called reverse transcriptase to make a copy of its RNA, but the copy is made as deoxyribonucleic acid that contain the code for a specific protein that functions in one or more types of cells in the body. Chromosomes are structures within cells… read more ). HIV mutates easily at this point because reverse transcriptase is prone to making errors during the conversion of HIV RNA to DNA. These mutations make HIV more difficult to control because the many mutations increase the chance of producing HIV that can resist attacks by the persons immune system and/or antiretroviral drugs.
Don’t Miss: Youngboy Has Herpes
Innate Immune Response To Hiv
Innate immune cells are the first line of defence which HIV encounters upon entry to the body.
Macrophages. Tissue macrophages are one of the target cells for HIV. These macrophages harbour the virus and are known to be the source of viral proteins. However, the infected macrophages are shown to lose their ability to ingest and kill foreign microbes and present antigen to T cells. This could have a major contribution in overall immune dysfunction caused by HIV infection.
Dendritic cells . DCs are large cells with dendritic cytoplasmic extensions. These cells present processed antigens to T lymphocytes in lymph nodes. Epidermal DCs, expressing CD1a and Birbeck granules, are probably among the first immune cells to combat HIV at the mucosal surfaces. These cells transport HIV from the site of infection to lymphoid tissue. The follicular DCs, found in lymphoid tissue, are also key antigen-presenting cells that trap and present antigens on their cell surfaces. In the lymph node follicles, DCs provide signals for the activation of B lymphocytes.
How Common Is Hiv
The number of people living with HIV in the UK continues to rise. This is because more cases are being diagnosed and people are living longer due to more effective medication
The most recent statistics on the number of people in Northern Ireland living with HIV are available from the Public Health Agency website.
You May Like: How Long Does Hiv Take To Show
Which Cells Are Destroyed By Hiv
The last stage of HIV infection is AIDS .The antiretroviral treatment used today is designed to block HIV infection, the main targets of HIV. This could be a step towards possible remission through the elimination of reservoir cells for people living with HIV.Which of the following T-cells are destroyed by HIV? 000+ LIKES, Join the 2 Crores+ Student community now, Nucleocapsids containing viral genome and enzymes enters the target cell .Role of CD4 T-Cells in HIV Infection , but precisely how these cells are killed has not been clear, the virus continues to stay inside the body and make use of the cells metabolic and energy-producing qualities, a type of white blood cell that is vital to fighting off infection, From here, When the quantity of T cells drops below 200 per µL of blood the destruction of T4 lymphocytes, Khalili said, HIV infects and destroys certain white blood cells called CD4+ cells, If too many CD4+ cells are destroyed, 57: HIV and AIDS Biology LibreTexts> HIV infects only the CD4 cells of the immune system, are destroyed, [Photo: Chris Goodfellow, ex vivo.