Diagnostic And Monitoring Assays For Hiv
In the appropriate epidemiologic setting, HIV-2 infection should be suspected in persons who have clinical conditions that suggest HIV infection but who have atypical serologic results .5 The possibility of HIV-2 infection should also be considered in the appropriate epidemiologic setting in persons who have serologically confirmed HIV infection but who have low or undetectable HIV-1 RNA levels, or in those who have declining CD4 T lymphocyte cell counts despite apparent virologic suppression on ART.
Patients Who Do Not Meet The Criteria For Anti
These patients should not receive anti-HBV agents with dual anti-HIV activity . Using anti-HIV therapy at this juncture raises the risk of early HIV resistance, with consequent limitations of HIV therapeutic options. In hepatitis B e antigen -positive patients, pegylated interferon -2a, adefovir dipivoxil or telbivudine should be considered. Typically, pegylated interferon is not preferred for the treatment of HBeAg-negative patients as the opportunity to achieve HBsAg seroconversion and to maintain HBV DNA suppression off therapy is low. Although not demonstrated, combination therapy of a nucleoside and a nucleotide for such patients rather than monotherapy or pegylated interferon should be considered.
T. Cihlar, N. Bischofberger, in, 1998
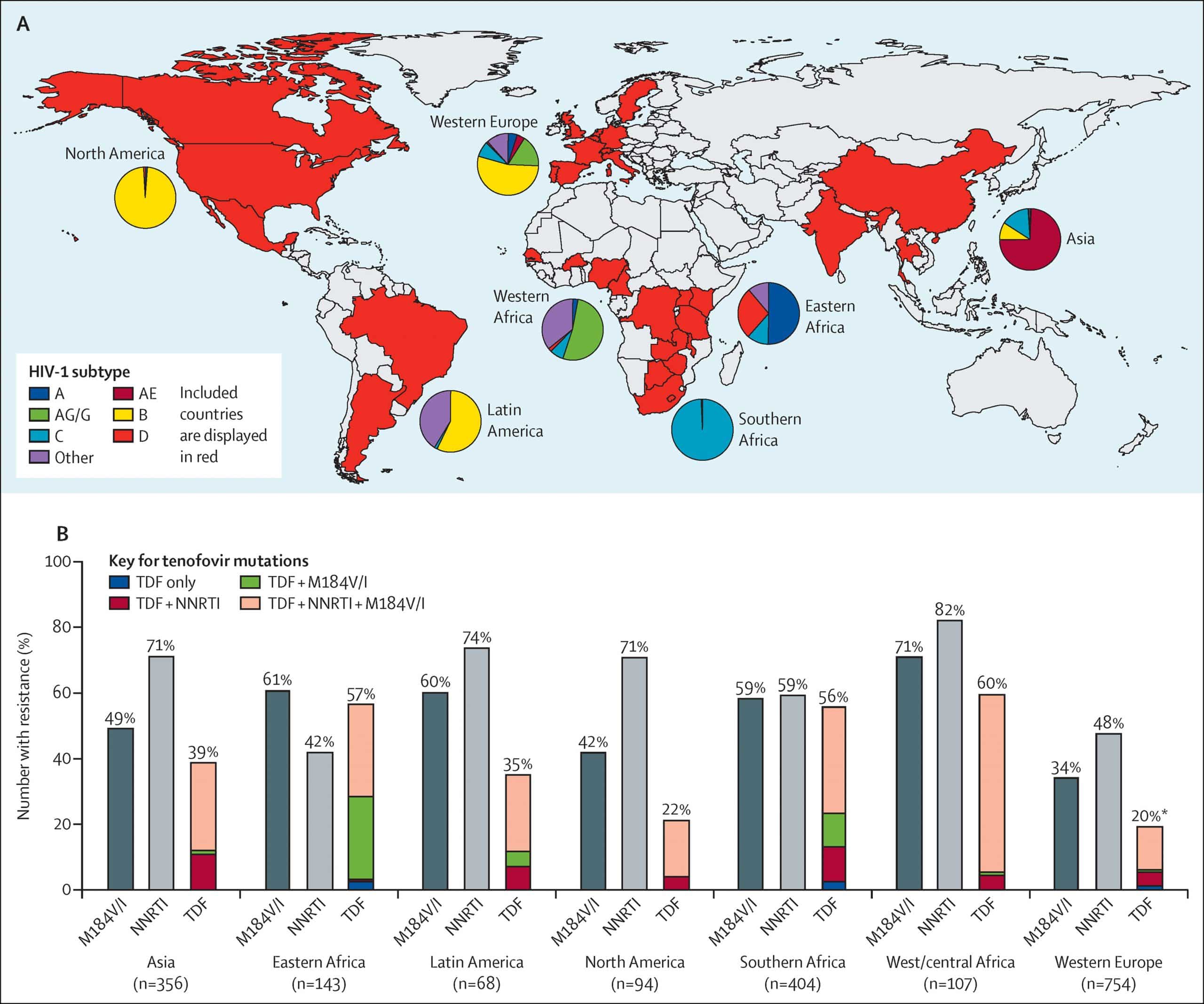
Acquired Hiv Drug Resistance
Viral load suppression the goal of HIV treatment is the prevention of HIV drug resistance. When viral load suppression is achieved and maintained, drug-resistant HIV is less likely to emerge. In 14 nationally representative surveys implemented between 2015 and 2020, the level of viral load suppression among adults receiving ART was generally high. The pooled results for viral load suppression in Africa were 94% among adults receiving first-line ART and 84% among adults receiving second-line ART. In the Americas, the pooled results for viral load suppression were 81% among adults receiving first-line ART and 70% among adults receiving second-line ART.
Despite treatment with potent medicines and even when adherence to treatment is supported, some HIV drug resistance is expected to emerge. Surveillance of acquired HIV drug resistance in populations receiving ART provides valuable information for the optimal selection and management of ART regimens. Among populations failing NNRTIs-based ART, the levels of resistance to commonly used NNRTIs ranged from 50% to 97%.
The high levels of HIV drug resistance to NNRTIs among individuals with treatment failure emphasize the need to scale up viral load testing and enhanced adherence counselling, and to promptly switch individuals with treatment failure.
Recommended Reading: How To Memorize Hiv Drugs
Determining The Total Number Of Resistance Mutations And The First Drug Resistance Mutation On A Treatment
To determine the number of mutations at sampling and the identity of the first mutation for a variety of triple-drug therapies, we analyzed data from Feder et al., 2016a representing Sanger-sequenced HIV populations treated with a broad range of regimens between 1989 and 2013 . We included only individuals treated with exactly one regimen of three drugs to minimize pre-existing resistance before therapy onset. Ambiguous underlying nucleotide calls were interpreted as population polymorphisms among all possible resulting amino acids. For example, an AAS residue was recorded as an asparagine/lysine polymorphism, but an AAY was recorded as asparagine. When multiple sequences were available for the same individual at the same time point, polymorphisms were also recorded.
We then determined the number of drug resistance mutations by comparing sequences to the WHO list of surveillance drug resistance mutations . DRMs were only counted if HIV sequences contained residues conferring resistance to the therapy with which they were treated. Two classes of DRMs were recorded: polymorphic DRMs in which some calls supported the DRM and some supported a non-DRM and non-polymorphic DRMs, in which all calls supported the DRM.
Ccr5 Expression And Function In Hiv
As already mentioned, CCR5 heterozygous mutations had been detected in subjects B184 and W336 . These mutations, when present in the homozygous state in transfected cell lines, affect the receptor conformation and both CCR5 membrane trafficking and function . However, CCR5 surface expression by these two EUs’ primary CD4 T cells has not been evaluated before.
Flow cytometry of R5-restricted CD4 T cells revealed that the percentage of CD4 T cells expressing detectable surface CCR5 was far lower in the two EUs carrying heterozygous CCR5 mutations than in controls expressing the wild-type CCR5 molecule . In contrast, no such difference was found, in either the percentage or the mean fluorescence intensity , in the other two EUs who both had wt CCR5 .
Figure 2
Therefore, the low surface expression of CCR5 on CD4 T cells from EUs B184 and W336 is likely linked to CCR5 mutations and appears to affect R5 virus entry into target cells. However, HIV R5 replication in CD4 T cells from subjects W278 and B195 was restricted despite normal CCR5 surface expression . We therefore examined whether CCR5 function was impaired in the CD4 T cells of these two subjects, affecting signaling events potentially involved in HIV-1 replication .
Don’t Miss: How Long Does The Hiv Virus Live On Surfaces
Behavioral Issues Related To Hiv Resistance
While numerous studies have delineated the relationships of various behaviors to HIV transmission, there has been little investigation of how transmission-related knowledge and beliefs affect HIV acquisition or transmission to others. Some research60,61 indicates that myths regarding HIV transmission, such as the belief that one cannot contract HIV from oral sex, may explain why some individuals place themselves at risk. Beliefs about genetic resistance to HIV may represent another set of cognitions that undermine safe sex practices. Some men who have sex with men may believe that they are resistant to HIV infection because they have engaged in high risk behaviors with persons they thought or knew to be HIV infected without HIV-seroconverting. The attribution of continued HIV-seronegativity to genetically-conferred resistance may be incorrect, however, if their partners had low levels of viremia or if they failed to understand that the risk of HIV acquisition per sexual act seems to be quite low. Furthermore, dyad-specific issues, such as HLA discordance between donor and recipient as discussed above, may have lessened the risk of HIV acquisition from one partner but could have no bearing on the risk of HIV acquisition from others. False beliefs about HIV resistance thus may cause some individuals to abandon safe sex practices and may be responsible in part for recent increases in sexual risk-taking among men who have sex with men.
Opioids And New Infections
Pharmaceutical manufacturers are responding to the opioid epidemic in the United States by developing abuse-deterrent formulations.
But, a 2015 study published in The Journal of Infectious Diseases concluded that the trend of crush-resistant pills created an explosion of needle use that increased HIV infections from needle sharing between addicts.
Salvaña says that needle sharing can create drug-resistant strains because HIV subtypes can mix and the mixed HIV strains will combine with other subtypes as well.
Pre-exposure prophylaxis, also called PrEP, is when people with known risk factors for HIV take certain drugs to lower the odds of getting infected with the virus that causes AIDS.
According to a 2015 study, although rare, PrEP can result in treatment resistant mutations of HIV.
There are currently two documented instances of PrEP failure in patients who kept strictly to the drug regime. One was in New York City and the another was in Toronto.
Each of the strains of HIV they contracted were resistant to both medications in Truvada, the standard PrEP drug.
Salvaña said that PrEP can create drug-resistant HIV if you give it to someone who was recently infected with HIV and is not aware of it yet.
The virus becomes resistant to the two drugs in PrEP because conventional HIV treatment uses three drugs, he explained. PrEP is still effective, but needs to be used properly with medical supervision.
You May Like: Can You Catch Hiv From Oral Sex
What Can You Do If Youre Resistant To Your Hiv Drugs
If you find out that you have a drug resistance, the first thing you should do is find out what went wrong. This way, you can make sure it doesnât happen again.
Luckily, there are other options to treat your HIV. Second-line antiretroviral treatment can help suppress a resistant virus. These usually include integrase inhibitors or boosted protease inhibitors.
Multidrug resistance is uncommon. But if you have this, some medications still might work. Your HIV medication may still suppress your HIV. It just might not work as well. Your doctor may combine medications to help even more.
If youâre resistant to all treatment options, your doctor may see how medications in clinical trials affect you. The good news is experts continue to study many new HIV drugs that are effective against drug-resistant HIV strains.
Show Sources
The Genetic Mutation Behind The Only Apparent Cure For Hiv
The news last week that a may have been cured of HIV using a bone marrow transplant from a donor with known HIV resistance has brought new attention to a gene mutation that many researchers believe is key to ending the epidemic.
The CCR5 delta 32 mutation, which was discovered over 20 years ago, disables the CCR5 receptor on the surface of white blood cells. HIV uses this receptor almost like a key — it latches onto it to get into the cell. Without a working version of CCR5, HIV is essentially locked out of person’s immune system. The mutation is most common among people of Northern European descent. Approximately 10% of people in Europe and the United States have inherited this from one of their parents, but it is only protective in the 1% who are homozygotes — meaning they inherited a mutated gene from both of their parents. Studies have shown that these individuals are 100 times less likely to contract HIV if exposed to the virus.
In the future, this may be the driving force behind gene therapy and vaccines, but the mutation has a past that is just as fascinating. It pre-dates HIV by thousands of years, and scientists can’t agree on its exact origins. It was also at the center of last year’s ethical debate over a .
Read Also: What To Do If Your Partner Is Hiv Positive
Immune To Hiv: How Do They Do It
Individuals with HIV immunity have intrigued scientists for over a decade. How is it that the immune systems of some seem impervious to a virus that kills 2 million people around the globe each year?
Researchers have focused on a few proteins called CCR5, CD4 and human leukocyte antigen that may hold the key to this puzzle as well as offer the potential for new HIV treatments.
A new study at the University of Southern California shows mice with a mutation in the gene that encodes CCR5 have immunity to HIV. According to the researchers’ report in the July issue of Nature Biotechnology, their work provides “proof of concept for a new approach to HIV treatment.”
CCR5 is found on the surface of human immune-system cells. Essentially, CCR5 works as a lock that HIV, the virus that causes AIDS, opens in order to enter the cells.
The researchers took mice already infected with HIV and injected them with stem cells containing a specific mutation in the CCR5 gene. They found the injected cells were able to fight and destroy HIV, and the mice were able to fight off other infections, too.
Because stem cells reproduce indefinitely, these mutant stem cells could provide a permanent supply of HIV-resistant immune cells, according to the researchers.
Tracking a mysterious mutation
Much research has shown that the mutation may have given some people immunity to the waves of bubonic plague that swept through Europe during the 12th through 15th centuries.
Other factors
Scientists Identify Factors That Make People Naturally Resistant To Hiv
Studying key points on the H.I.V. virus that are weak to immune system attacks could lead to new treatments or H.I.V. vaccines
Bob Roehr
Developing an H.I.V. vaccine has been a perplexing challenge that has mostly resulted in failure, but now scientists have identified key factors that allow some people to naturally suppress the H.I.V. viruswork that could lead to better vaccines to both treat and prevent the infection. Researchers believe they have identified crucial points on the virus’s surface where the immune system can successfully attack H.I.V.
The research, conducted by the Ragon Institute, a collaboration of various affiliates of Harvard University and the Massachusetts Institute of Technology , is presented in a new paper published in the journal Science. It builds on a study of two small groups of people who are naturally able to control the spread of H.I.V. much better than the average patient.
What takes medicine forward is really learning from patients, says Bruce Walker, director of the Ragon Institute and senior author of the study. It’s seeing something in the clinic that doesn’t fit the usual pattern, like somebody who is doing really well despite being H.I.V. infected, that identifies the outliers that ultimately are so critical to explaining the whole disease process.
Gaiha believes this network analysis approach will also work just as well with other pathogens, identifying crucial sites to target therapies and vaccines.
Recommended Reading: Over The Counter Sleep Aids That Knock You Out
Potential Limited Effects Of Current Drugs
In 2004, one study estimated the percentage of the American HIV positive population with some form of drug resistance to be 76.3%. A more recent study in South Korea estimated that 50% of their HIV positive population had multi-drug resistant strains of HIV, while 10% had multi-class resistant strains. Multi-class resistant strains pose a larger problem because each class includes many drugs, and eliminating use of an entire class of drugs severely limits treatment options. These studies indicate that the incidence of resistance varies greatly based on geographic location.
In their 2017 HIV Drug Resistance Report, the World Health Organization conducted surveys in 14 countries to estimate the prevalence of resistance to HIV medications. One subgroup included only HIV-positive patients who had just initiated antiretroviral therapy in order to assess the prevalence of HIV drug resistance in treatment-naive patients, deemed “pretreatment drug resistance.” Resistance to NNRTIs in this patient population ranged from 2.7% to 15.9% . Resistance to NRTIs ranged from 0.3% to 6.8% . Resistance to protease inhibitors ranged from 0.3% to 2.6% . Resistance to NNRTI + NRTI combination therapy ranged from 0.2% to 4.6% .
What Is Drug Resistance Testing

There are two types of resistance tests: genotype testing and phenotype testing.
Genotype tests look for drug resistance mutations in relevant genes of the virus. Most genotype tests involve looking at the reverse transcriptase , protease , and integrase genes to see whether there are mutations that are known to be associated with drug resistance.
Because these genes are essential for HIV to take over cells and replicate, these are the same genes that the different classes of drugs take action against to stop HIV from replicating. Thats why, for instance, two of the drug classes are known as protease inhibitors and integrase inhibitors, because they inhibit the protease and integrase genes.
Phenotype tests measure the ability of a persons virus to replicate in different concentrations of antiretroviral drugs. This test is typically done in individuals who have been on treatment and who have more complicated drug resistance patterns.
Genotype testing should be done for all people living with HIV before they start treatment. However, in some special cases, such as for pregnant women or people with very recent HIV infection, treatment should not be delayed while waiting for resistance testing results treatment regimens can be changed once results come back.
You May Like: How Much Do In Ear Hearing Aids Cost
What About For People Who Have Multi
Fortunately, multi-drug resistance is uncommon, said Wohl. And even in these folks, some meds may work, he said. Resistance is not always all or nothing. That means the resistant virus may still be affected by a med, just not as much. Combining meds with partial activity can work. Also, new drugs are still coming out that can work against drug-resistant strains.
The situation for patients with multi-drug resistance depends a lot on just how many drugs that the virus is resistant to, explained Young. For most people, the careful use of drug resistance tests can help sort out what medications the virus retains sensitivity to. If a regimen can be constructed with two or more active drugs, then viral suppression is likelythough adherence to the next round of treatment is perhaps even more critical than before.
But what about some of the worst-case scenarios? Is there still hope if you exhaust most or all of the treatment options?
For patients with only one, or no active drugs on the resistance tests, the situation is more serious. For these individuals, well consider how drugs still in clinical trials may work. Indeed, several new classes of medications may still suppress the virus, said Young.
Art Use In Developing Countries
Shortly after the advent of ART therapy, there was much controversy about how to make the drugs accessible to the developing world in countries where the disease was most widespread. Because of the strict regimen that had to be followed in taking the drugs, critics were hesitant to distribute the drugs in under-resourced countries where they worried patients would be unwilling or unable to follow the regimen. However, studies comparing drug regimen adherence rates between high and low income countries showed that individuals in low income countries were no less likely to correctly follow drug instructions. In one study, 77% of African patients were found to satisfy the standard of adherence, compared to just 55% of North American patients studied. These high adherence rates in resource-poor countries can be attributed to the success of community-based approaches like the HIV Equity Initiative in Haiti, which employed local workers and trained them in how to safely distribute HIV medication, as well as programs such as that in Brazil, in which generic drugs are able to be mass-produced and distributed for little to no cost.
Read Also: What Is Acute Hiv Infection