An International Research Group With Essential Participation Of The Paul
HIV-1 uses human proteins for its own replication and prevents the human immune system from combating it successfully. Dr Renate König, head of the research group Cellular Aspects of Pathogen Host Interactions of the Paul-Ehrlich-Institut, and her colleagues have been studying this phenomenon for a long time, asking why the human immune system fails to fight HIV-1. To identify the underlying reason could help develop both enhancers for future efficacious vaccines and new immune-modulated HIV antivirals. The researchers have now reached one important milestone toward achieving this goal in an international research collaboration with Dr Jenny Ting, University of North Carolina at Chapel Hill, NC, USA, and Dr Sumit Chanda, Sanford-Burnham Prebys Medical Discovery Institute, San Diego, CA. They have identified NLRX1 as an important factor. This protein belongs to the NOD-like receptor family of pattern recognition receptors. It acts as a fine-tuning regulator, which can deactivate the early warning system of the immune system. In a high-throughput procedure, NLRX1 had already been identified by König and colleagues as one out of 295 potential proteins important for HIV-1 replication . The fact that it does play a central role, and which mechanisms it uses, has so far been unknown.
How Hiv Disables Immune Cells
In order to be able to ward off disease pathogens, immune cells must be mobile and able to establish contact with each other. Professor Dr. Oliver Facklers group of researchers in the Department of Virology of the Institute of Hygiene at the University of Heidelberg has discovered a mechanism in an animal model revealing how HI viruses cripple immune cells: The mobility of cells is inhibited by the protein Nef. The study, which was published in the highly renowned journal Cell Host & Microbe, might potentially also open up new therapeutic strategies.
More than 30 million people worldwide are infected with HIV. Typically, the initial infection is accompanied by acute symptoms and then is followed by a latency period of several years before the acquired immunodeficiency syndrome manifests. The HI virus has developed numerous strategies for eluding the bodys immune defence as well as the effect of the drugs used to treat the infection. The viral Nef protein is a major prerequisite for the efficient reproduction of the virus in the affected individuals. The development of AIDS is significantly slowed without Nef, or even stops completely. The underlying mechanism of this observation has, however, previously not been known.
Scientists Uncover How Hiv Evades Elimination By The Immune System
Posted: 20 April 2018 | Drug Target Review |
A team of scientists from Trinity College Dublin has identified the mechanism that enables HIV to evade the immune system, paving the way for a new curative treatment.
The new research shows that HIV targets and disables a pathway involving a number of biological molecules that are fundamental in blocking viral activity and clearing infection, illustrating precisely how the virus avoids elimination.
HIV remains a major global health problem, with over 40 million people infected worldwide. Whilst people living with the virus have been treated with anti-retroviral therapy for over 30 years, this favoured therapeutic option merely prevents the progression of the disease to AIDS it doesnt provide a cure. The discovery of this mechanism represents a major step forward in the quest to develop an effective treatment for the virus and opens the door to a new era of research in this area.
During any viral infection our immune system produces a powerful molecule , which interferes with the infection and the replication of viruses. Interferon activates an assembly line of molecules in our cells via the interferon signalling pathway which causes the body to make antivirals that help to clear the infection.
The study was published in EBioMedicine.
Related topics
Recommended Reading: How Do You Get Hiv 2
Researchers Uncover How Ebola Virus Disables Immune Response
by Cell Press
One of the human body’s first responses to a viral infection is to make and release signaling proteins called interferons, which amplify the immune system response to viruses. Over time, many viruses have evolved to undermine interferon’s immune-boosting signal, and a paper published today in the journal Cell Host & Microbe describes a mechanism unique to the Ebola virus that defeats attempts by interferon to block viral reproduction in infected cells.
The newly published study explains for the first time how the production by the virus of a protein called Ebola Viral Protein 24 stops the interferon-based signals from ramping up immune defenses. With the body’s first response disabled, the virus is free to mass produce itself and trigger the too-large immune response that damages organs and often becomes deadly as part of Ebola virus disease .
The study was led by scientists from Washington University School of Medicine in St. Louis in collaboration with researchers from the Icahn School of Medicine at Mount Sinai and the University of Texas Southwestern Medical Center.
Ebola Defeats Immune Defenses Early in Infection
The study spotlights the part of the body’s defense system that fights infection called innate immunity, the mix of proteins and cells that most quickly recognizes an invasion by a virus. This part of immunity keeps a virus from quickly reproducing inside cells.
Explore further
Evasion Of The Immune System By Pathogens
It is important to keep in mind that although the immune system has evolved to be able to control many pathogens, pathogens themselves have evolved ways to evade the immune response. An example already mentioned is in Mycobactrium tuberculosis, which has evolved a complex cell wall that is resistant to the digestive enzymes of the macrophages that ingest them, and thus persists in the host, causing the chronic disease tuberculosis. This section briefly summarizes other ways in which pathogens can outwit immune responses. But keep in mind, although it seems as if pathogens have a will of their own, they do not. All of these evasive strategies arose strictly by evolution, driven by selection.
Bacteria sometimes evade immune responses because they exist in multiple strains, such as different groups of Staphylococcus aureus. S. aureus is commonly found in minor skin infections, such as boils, and some healthy people harbor it in their nose. One small group of strains of this bacterium, however, called methicillin-resistant Staphylococcus aureus, has become resistant to multiple antibiotics and is essentially untreatable. Different bacterial strains differ in the antigens on their surfaces. The immune response against one strain does not affect the other; thus, the species survives.
Don’t Miss: How Fast Does Hiv Spread In The Body
Hiv Modifies The Cell Structure System Of The Host Cells
Viruses alter the support structure of affected cells in turn enabling them to enter the cells more easily. The cell structure element actin, which also gives muscles their mobility, aids in the motility of immune cells. The mobility is necessary for immune cells to be able to establish contact with each other and ward off the virus. After each movement, actin must be returned to its original state in order to be available again. HIV preferentially attacks the immune cells of the T-helper cell type. These cells support not only the direct defence mounted against the enemy, but are also necessary for producing sufficient antibodies against the invader. In order to do so, they must rely on their mobility.
How Is The Immune System Activated
The immune system can be activated by a lot of different things that the body doesnt recognize as its own. These are called antigens. Examples of antigens include the proteins on the surfaces of , fungi and viruses. When these antigens attach to special receptors on the immune cells , a whole series of processes are triggered in the body. Once the body has come into contact with a disease-causing germ for the first time, it usually stores information about the germ and how to fight it. Then, if it comes into contact with the germ again, it recognizes the germ straight away and can start fighting it faster.
The bodys own cells have proteins on their surface, too. But those proteins dont usually trigger the immune system to fight the cells. Sometimes the immune system mistakenly thinks that the body’s own cells are foreign cells. It then attacks healthy, harmless cells in the body. This is known as an autoimmune response.
Also Check: What City Has The Highest Hiv Rate
Innate Immune Response To Hiv
Innate immune cells are the first line of defence which HIV encounters upon entry to the body.
Macrophages. Tissue macrophages are one of the target cells for HIV. These macrophages harbour the virus and are known to be the source of viral proteins. However, the infected macrophages are shown to lose their ability to ingest and kill foreign microbes and present antigen to T cells. This could have a major contribution in overall immune dysfunction caused by HIV infection.
Dendritic cells . DCs are large cells with dendritic cytoplasmic extensions. These cells present processed antigens to T lymphocytes in lymph nodes. Epidermal DCs, expressing CD1a and Birbeck granules, are probably among the first immune cells to combat HIV at the mucosal surfaces. These cells transport HIV from the site of infection to lymphoid tissue. The follicular DCs, found in lymphoid tissue, are also key antigen-presenting cells that trap and present antigens on their cell surfaces. In the lymph node follicles, DCs provide signals for the activation of B lymphocytes.
Pathogens Have Evolved Various Means Of Evading Or Subverting Normal Hostdefenses
Just as vertebrates have developed many different defenses against pathogens, sopathogens have evolved elaborate strategies to evade these defenses. Many pathogensuse one or more of these strategies to evade the . At the end of thischapter we will see how succeeds in defeating the by usingseveral of them in combination.
Read Also: How To Know If You Hiv
The Immune Response Against Pathogens
- Explain the development of immunological competence
- Describe the mucosal immune response
- Discuss immune responses against bacterial, viral, fungal, and animal pathogens
- Describe different ways pathogens evade immune responses
Now that you understand the development of mature, naïve B cells and T cells, and some of their major functions, how do all of these various cells, proteins, and cytokines come together to actually resolve an infection? Ideally, the immune response will rid the body of a pathogen entirely. The adaptive immune response, with its rapid clonal expansion, is well suited to this purpose. Think of a primary infection as a race between the pathogen and the immune system. The pathogen bypasses barrier defenses and starts multiplying in the hosts body. During the first 4 to 5 days, the innate immune response will partially control, but not stop, pathogen growth. As the adaptive immune response gears up, however, it will begin to clear the pathogen from the body, while at the same time becoming stronger and stronger. When following antibody responses in patients with a particular disease such as a virus, this clearance is referred to as seroconversion . Seroconversion is the reciprocal relationship between virus levels in the blood and antibody levels. As the antibody levels rise, the virus levels decline, and this is a sign that the immune response is being at least partially effective .
Everyday Connection: DisinfectantsFighting the Good Fight?
The Acquired Immune System
The acquired immune system, with help from the innate system, produces cells to protect your body from a specific invader. These antibodies are developed by cells called B lymphocytes after the body has been exposed to the invader. The antibodies stay in your child’s body.;It can take several days for antibodies to develop. But after the first exposure, the immune system will recognize the invader and defend against it. The acquired immune system changes throughout your child’s life. Immunizations;train your child’s immune system to make antibodies to protect him or her from harmful diseases.
The cells of both parts of the immune system are made in various organs of the body, including:
-
Adenoids. Two glands located at the back of the nasal passage.
-
Bone marrow. The soft, spongy tissue found in bone cavities.
-
Lymph nodes. Small organs shaped like beans, which are located throughout the body and connect via the lymphatic vessels.
-
Lymphatic vessels. A network of channels throughout the body that carries lymphocytes to the lymphoid organs and bloodstream.
-
Peyer’s patches. Lymphoid tissue in the small intestine.
-
Spleen. A fist-sized organ located in the abdominal cavity.
-
Thymus. Two lobes that join in front of the trachea behind the breastbone.
-
Tonsils. Two oval masses in the back of the throat.
Don’t Miss: Can You Contract Hiv From Someone Who Is Undetectable
Hiv And Immune System
- HIV eventually destroys many of the white blood cells, which protect us against disease.
- HIV infection leaves people helpless against many other serious infections and cancers.
T-cells and HIV infection
- There is a significant drop in number of circulating CD4 T cells at this early stage.
- An immune response to HIV occurs 1 week to 3 months after infection, when the levels of CD4 cell increases. But the immune response is unable to clear the infection completely, and HIV-infected cells persist in the lymph nodes.
- This period of clinical latency may last for as long as 10 years. Although very few infected cells are in the blood.
- HIV found in patients with late-stage disease is usually much more virulent and harmful than the strains of virus found early in infection.
Further Reading:
- AIDS infected persons show an abnormal B cell function.
- It produces an inability to mount an adequate immunoglobulin M response against the HIV.
Monocytes and HIV:
How Ebola Virus Disables The Body’s Immune Defenses

- Date:
- University of Texas Medical Branch at Galveston
- Summary:
- A new study uncovered new information on why the Ebola virus can exert such catastrophic effects on the infected person. They’ve described for the first time how the virus disables T cells, an important line of immune defense, thus rendering the infected person less able to combat the infection.
A new study by researchers from The University of Texas Medical Branch at Galveston uncovered new information on why the Ebola virus can exert such catastrophic effects on the infected person. They’ve described for the first time how the virus disables T cells, an important line of immune defense, thus rendering the infected person less able to combat the infection. The findings are currently available in PLOS Pathogens.
Ebola virus disease is one of the most devastating infectious diseases known to exist, with previous outbreaks resulting in high fatality rates. The particularly aggressive nature of Ebola virus stems from its ability to rapidly disarm the infected person’s immune system by blocking the development of a virus-specific adaptive immune response.
White blood cells are an important part of our immune system. Lymphopenia happens when the white blood T cell count in the bloodstream is lower than normal — in fact, the extent of lymphopenia is one of the strongest indicators of how severe the Ebola infection will become.
Story Source:
Recommended Reading: What Do Hiv Bumps Look Like
The Mucosal Immune Response
Mucosal tissues are major barriers to the entry of pathogens into the body. The IgA antibodies in mucus and other secretions can bind to the pathogen, and in the cases of many viruses and bacteria, neutralize them. Neutralization is the process of coating a pathogen with antibodies, making it physically impossible for the pathogen to bind to receptors. Neutralization, which occurs in the blood, lymph, and other body fluids and secretions, protects the body constantly. Neutralizing antibodies are the basis for the disease protection offered by vaccines. Vaccinations for diseases that commonly enter the body via mucous membranes, such as influenza, are usually formulated to enhance IgA production.
Immune responses in some mucosal tissues such as the Peyers patches in the small intestine take up particulate antigens by specialized cells known as microfold or M cells . These cells allow the body to sample potential pathogens from the intestinal lumen. Dendritic cells then take the antigen to the regional lymph nodes, where an immune response is mounted.
Study Identifies How Suppressed Hiv Keeps Immune System On Edge
By Brandon Levy
Tuesday, April 27, 2021
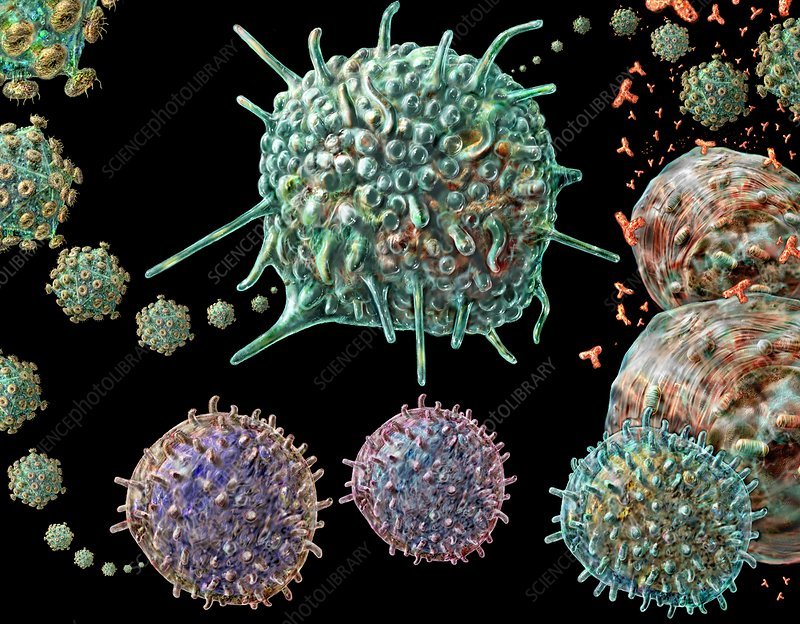
HIV needs to activate immune cells like this one to infect them. New IRP research identified how the virus continues to stimulate the immune system even when fully suppressed by antiretroviral therapy.
Over the four decades since it mysteriously began destroying the immune systems of Americans in New York and California, HIV has proven to be a frustratingly wily opponent for scientists. Even today, when treatments can fully suppress the virus in infected individuals, it continues to harm their health. A new IRP study has identified several ways dormant HIV might chronically stimulate the immune system, suggesting potential avenues for preventing the health problems that causes.1
Doctors have been using antiretroviral therapy to treat HIV for more than 30 years, forcing the virus into an inactive state in the body and turning what was once a death sentence into a manageable, chronic condition. However, over that long time period, they began to notice that people living with successfully suppressed HIV infections were developing age-related ailments like cardiovascular and kidney disease and neurological problems noticeably earlier in life than the general population.
Antiretroviral drugs like these can completely stop HIV from replicating in the human body, but do not stop the dormant virus from activating the immune system.
More From the IRPHIV Research Yields an Unexpected Discovery
References:
Don’t Miss: How Does Hiv Affect People
Molecular Mechanisms To Control Hiv Infection
Host cells can produce antiviral factors in an effort to eliminate invading HIV1. Although HIV can express its own factors to counteract these antiviral mechanisms, immune cell-intrinsic factors, including A3G, MX2 and RIG-I, which are discussed below, still play important roles in combating HIV infection.
The antiviral factor APOBEC3G enhances the recognition of HIV-infected primary T cells by natural killer cells8 Nature Immunology
HIV-infected T cells utilize the antiviral factor APOBEC3G , a cytidine deaminase that causes guanosine-to-adenosine hypermutation in HIV, resulting in inactivation of the virus. Interestingly, Norman et al. found that A3G also upregulates the expression of NK cell-activating ligands, NKG2D ligand, and thus enhances NK cell cytotoxicity towards HIV-infected T cells. This study describes how NK cells can detect HIV-infected T cells to help eliminate them.
MX2 is an interferon-induced inhibitor of HIV-1 infection9 Nature Letter
Type-I interferon , which includes IFN- and IFN-, is critical for antiviral responses. Here, the Bieniasz lab identified that myxovirus resistance 2 is an integral part of the IFN–induced antiviral response to HIV-1. MX2 is expressed in macrophages and CD4+ T cells, among other cell types, and its expression can be induced by exposure to IFN-. Mechanistically, this study suggests that MX2 inhibits the ability of HIV-1 to import its DNA into the nuclei of host cells.