How To Pay For Pep
Use the resources below to get help paying for PEP:
- Patient assistance programs. Many pharmaceutical companies have patient assistance programs that offer low-cost or no-cost medications to eligible individuals. Some to check out are:
- Gilead Advancing Access.Advancing Access is the patient assistance program from the producer of Truvada.
- Merck. Merck has patient assistance programs for many of their drugs, including Isentress.
- ViiV Connect.ViiV Connect is the patient assistance program from ViiV Healthcare, the maker of Tivicay.
Is The Prep Medication Effective For Treating Hiv Infection
PrEP medications are not effective alone for treating HIV infection. If you acquire HIV infection while taking PrEP, the provider who conducted the HIV test should either provide HIV medical care or refer you to a healthcare provider who can provide HIV care. The HIV care provider will conduct lab tests and determine the most effective regimen to treat your HIV infection. There is no evidence that having taken PrEP will impact the effectiveness of your HIV treatment. People who acquire HIV while on PrEP can be successfully treated with HIV medications.
If The Source Is Not Available
When the source of any potential exposure to HIV is not known, not available, or cannot be HIV tested for any reason, the care provider should assess the exposed individuals level of risk, assume the source has HIV until proven otherwise, and respond accordingly.
Determining whether the exposure warrants PEP and promptly initiating PEP when indicated should be the focus at initial presentation, rather than the HIV status of the source.
Also Check: Can You Get Hiv From Pedicure
Alternative Pep Regimens For Patients Who Weigh 40 Kg
Table 3, below, lists 2 alternative PEP regimens that are acceptable options when a preferred regimen is not available. They are possibly less well tolerated than the preferred regimen of TDF/FTC plus RAL or DTG, but they are significantly better tolerated than regimens containing ZDV or lopinavir/ritonavir . Observational studies have demonstrated excellent tolerability and completion rates .
A single-tablet regimen for a patient with adequate kidney function and no expected drug-drug interactions may be a good option for those who prefer a once-daily, single-tablet PEP regimen. It also allows use of medication assistance programs if a patient has limited medication coverage options.
Drug-drug interactions: The potential for drug-drug interactions in patients receiving PIs or cobicistat is increased due to the extensive cytochrome P450 interactions. Clinicians should assess for potential interactions before prescribing a PEP regimen.
| Table 3: Alternative PEP Regimens for Patients Who Weigh 40 kg |
|
|
| KEY POINT |
|
How Do I Use Pep
PEP is a course of daily pills you take over 28 days.
Once you finish your course of PEP, it is important to get an HIV test. You should get an HIV test at four to six weeks after you first started PEP and again three months after starting PEP. This is because it can take up to three months for HIV to show up on a test.
PEP is an emergency measure and isnt intended as a strategy to use regularly. If you dont always use condoms, talk to your doctor about using PrEP.
Also Check: How Many Pills Do Hiv Patients Take Daily
How Well Does Pep Work
PEP does not prevent 100% of HIV infections but it is very effective at preventing HIV if used consistently and correctly.
Observational research suggests that PEP can reduce the risk of getting HIV by more than 80%, which means some people in the studies acquired HIV despite taking PEP. Although some of these people reported high adherence to PEP and no further exposures to HIV, many HIV transmissions among people taking PEP occurred because of low adherence and/or ongoing exposures to HIV. Effectiveness is likely much higher than 80% if PEP is used consistently and correctly, as prescribed. This includes:
- Obtaining PEP from a healthcare provider.
- Taking the medications every day for 28 days. High adherence to the full month-long course of PEP is important for maximizing effectiveness.
- Starting PEP as soon as possible after a potential exposure to HIV, but not more than 72 hours afterwards. The sooner PEP is started after an exposure to HIV the more likely it is to work because the drugs need to start interrupting HIV replication as soon as possible.
- Taking extra precautions to reduce the risk of being exposed to HIV again while taking PEP. The use of PEP is meant to reduce the risk from a single exposure to HIV and should only be used for emergencies.
Whats The Difference Between Prep And Pep
If youve done any research on HIV prevention and treatments, you have probably seen the terms PrEP and PEP. While these two terms look quite similar they are very different and it is important that you understand what each of them mean.
Now first, lets go over the similarities of PrEP and PEP. Both are treatment plans intended for people who at high risk of HIV transmission but are currently negative for HIV. This could be:
- Someone who has had unprotected sex with a partner who has HIV or whose HIV status is unknown.
- Someone who has shared needles or drug preparation equipment with other people.
- Someone who has contracted an STD within the past six months.
Now, just because a person comes into contact with HIV does not automatically mean they will contract it. Since HIV is a virus, it is measured by the viral load in a persons bloodstream. Upon first contact, the viral load will be low and highly manageable. But if the virus is left untreated, the viral load will increase quite quickly, as you can see from the graph below.
So, it is incredibly important for a person to use proper protection measures and treatment plans to either prevent HIV transmission in the first place or treat it as soon as possible.
This is where PrEP and PEP fit in.
So, now lets explain the key differences between these HIV treatment and prevention plans.
Read Also: How Long Until You Test Positive For Hiv
How Effective Is It
Although not guaranteed to work, PEP is often a sensible idea and may help put your mind at rest. There have been a number of primate studies, in which animals were exposed to HIV and then PEP. Overall, the ones that received the PEP were 89% less likely to seroconvert than the ones that were given HIV alone.
Obviously, it would be an ethical minefield to conduct this kind of study in humans.
However, there is good evidence that it works in people too. In one 2005 study, 702 people were evaluated, all of whom had taken PEP after HIV exposure. After 12 weeks, only three had become HIV-positive .
While we don’t know how many would have seroconverted otherwise, the evidence suggests it would have been considerably higher than three. This implies the PEP prevented some cases of HIV.
How good is PEP for preventing HIV?
Management Of The Exposed Site
Care of the exposure site should prioritize appropriate cleansing and infection preventive measures and minimize further trauma and irritation to the exposed wound site. The site of a wound or needlestick injury should be cleaned with soap and water only. It is best to avoid use of alcohol, hydrogen peroxide, povidone-iodine, or other chemical cleansers. Squeezing the wound may promote hyperemia and inflammation at the wound site, potentially increasing systemic exposure to HIV if present in the contaminating fluid. The use of surgical scrub brushes or other abrasive tools should be avoided, as they can cause further irritation and injury to the wound site. Eyes and other exposed mucous membranes should be flushed immediately with water or isotonic saline.
Recommended Reading: Can You Get Hiv If You Only Have One Partner
When To Consult An Expert Regarding The First Dose Of Pep
Examples of clinical scenarios that warrant consultation with an experienced HIV care provider include: a source with ARV-resistant HIV, an exposed individual with limited options for PEP medications due to potential drug-drug interactions or comorbidities, or an exposed individual who is pregnant or unconscious.
Expert consultation for New York State clinicians: In such circumstances, clinicians are advised to call the Clinical Education Initiative to speak with an experienced HIV care provider.
The Clinical Consultation Center for PEP may be reached by calling 1-888-448-4911. The CCC is part of the AIDS Education and Training Centers and is located at the University of California, San Francisco/Zuckerberg San Francisco General Hospital. It is funded by the Health Resources and Services Administration and the Centers for Disease Control and Prevention. See UCSF > PEP for more information, including hours.
How Can People At High Risk Of Getting Hiv Access Prep
An HIV-negative person who wants to take PrEP needs to get a prescription from a provider who is willing to provide the necessary medical follow-up. PrEP does not need to be prescribed by an HIV specialist, but not all providers are knowledgeable about PrEP. Unfortunately, it may be difficult for clients to find a provider who is willing to prescribe PrEP.
The cost of TDF + FTC as PrEP is covered by most public and some private health insurance plans in Canada. Since TDF + FTC is available in generic drug formulations, this has brought down the cost to as low as about $250 a month, without insurance coverage. However, TAF + FTC is currently not covered by most public health insurance plans in Canada. Since TAF + FTC is only available as the brand name drug , it is much more expensive, around $1,000 to $1,200 a month.
You May Like: How Long Before Hiv Symptoms
Who Can Use Pep
PEP is for people who may have been exposed to HIV in the last 3 days. PEP might be right for you if:
-
You had sex with someone who may have HIV and didnt use a condom, or the condom broke
-
You were sexually assaulted
-
You shared needles or works with someone who may have HIV
If you were exposed to HIV in the last 3 days and want PEP, see a nurse or doctor or go to the emergency room immediately. Timing is really important. You must start PEP as soon as you can after being exposed to HIV for it to work.
PEP is for emergencies. It cant take the place of proven, ongoing ways to prevent HIV like using condoms, taking PrEP , and not sharing needles or works. If you know you may be exposed to HIV often , talk to your nurse or doctor about PrEP.
If youre a health care worker and think you may have been exposed to HIV at work, go to your doctor or the emergency room right away. Then report the incident to your supervisor. HIV transmission in health care settings is extremely rare, and there are procedures and safety devices that can lower your chances of coming into contact with HIV while caring for patients.
How Can People Access Pep

The Canadian PEP guidelines recommend that PEP should be readily available in places where it is likely to be needed urgently. These include emergency departments, sexual health clinics and other clinics serving populations at increased risk of HIV.
The decision to provide PEP lies with the healthcare provider and is made on a case-by-case basis. Many healthcare providers are unaware of non-occupational PEP or may be unwilling to prescribe it. The Canadian guidelines outline practical advice for physicians providing PEP, including how to assess risk in people who present for PEP, how to provide monitoring and follow-up, and recommended drug regimens.
People starting PEP may be offered a starter pack of pills, so that PEP can be started right away, along with a prescription that needs to be filled to receive the full 28-day course of medications. Most emergency departments will have PEP starter packs available.
Anti-HIV drugs are expensive: a month-long course of PEP can cost $900 or more, depending on the drugs used. Although occupational PEP is normally covered by workplace insurance, coverage for non-occupational PEP varies across Canada. Non-occupational PEP medications are covered by some private and public health insurance plans coverage varies depending on the province or territory and the type of exposure.
Acknowledgement
Also Check: Can You Get Hiv From Saliva
Purpose And Use Of This Guideline
This guideline was developed by the New York State Department of Health AIDS Institute for healthcare practitioners in any medical setting who manage the care of individuals who request post-exposure prophylaxis after a possible exposure to HIV. Despite the availability of prevention measures, exposures occur that pose the risk of transmission. Fortunately, with rapid initiation of PEP, infection can be blocked. Preventing new HIV infections is crucial to the success of New York States Ending the Epidemic Initiative.
HIV transmission can be prevented through use of barrier protection during sex , safer drug injection techniques, and adherence to universal precautions in the healthcare setting. HIV infection can also be prevented with use of antiretroviral medications taken as pre-exposure prophylaxis . After an exposure has occurred, HIV infection can be prevented with rapid administration of ARV medications as PEP. The first dose of PEP should be administered within 2 hours of an exposure and no later than 72 hours after an exposure.
Common Questions About Pep
Are there any side effects to PEP?
As with any medication, side effects are possible. HIV medications used or PEP are usually well tolerated but side effects may occur. Common side effects include fatigue, headaches, diarrhea, bloating, vomiting and nausea. Contact our medical professionals if your symptoms do not improve or significantly deteriorate.
How effective is PEP?
PEP is very effective in preventing infection after a potential exposure to HIV virus. However, treatment must begin within 72 hours of the potential exposure. Early treatment increases the likelihood of a successful outcome. Additional support is also available through our counseling services provided to the LGBTQ+ community regardless of HIV status.
What are the drugs used in PEP?
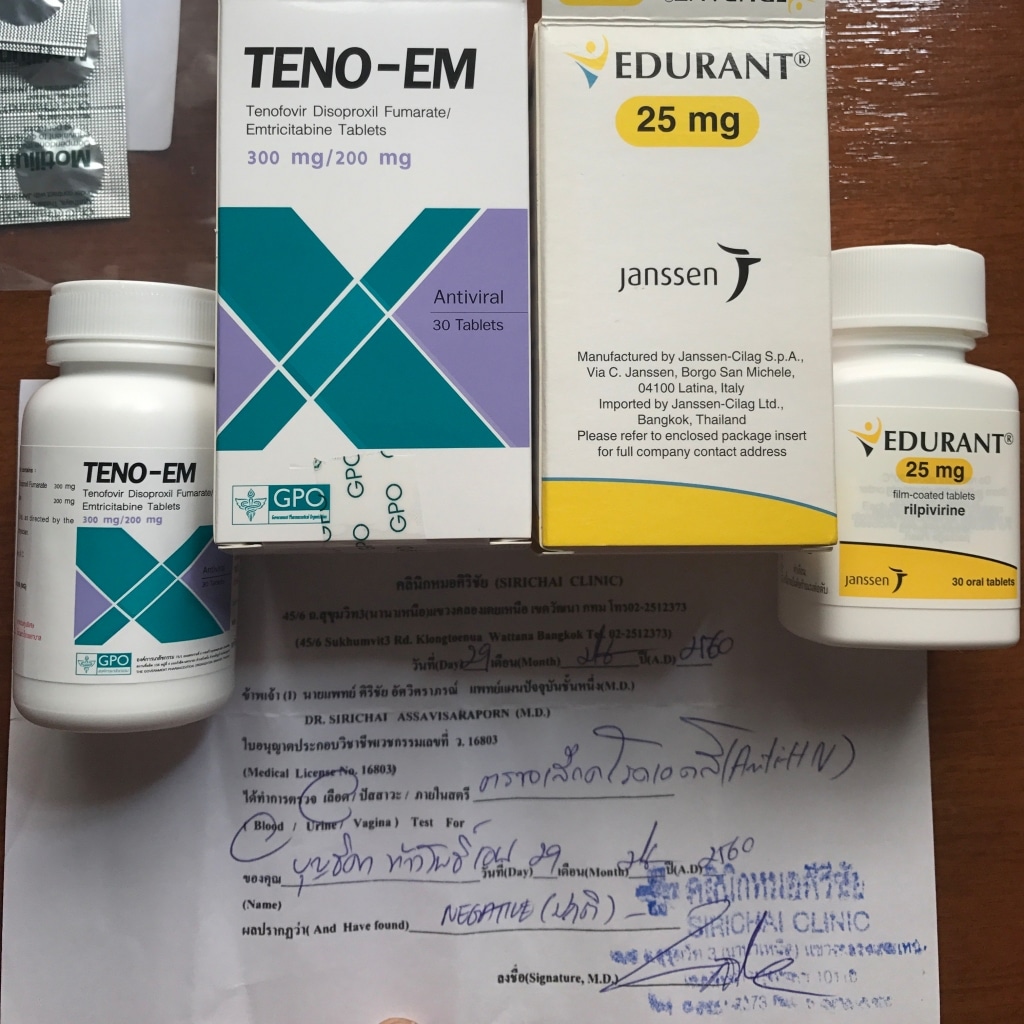
PEP requires individuals to take three drugs over 28 days. Some examples of regimens used are: Truvada and Isentress, Truvada and Tivicay, and Biktarvy. Our providers will consult with you what the best PEP option is or you.
Read Also: Best Hearing Aids For Young Adults
What Are Some Of The Safety Concerns Associated With Taking Pep
Drug resistance
A person with low adherence to PEP, who acquires HIV while taking PEP, could develop resistance to the drugs in PEP. If a persons HIV becomes resistant to the PEP drugs, those same HIV drugs may not work for treating their HIV.
Side effects
HIV drugs can cause side effects, such as nausea, fatigue and diarrhea. The nature and severity of the side effects depend on the type of drugs prescribed and the person who is taking them. The HIV drugs that are recommended for PEP in Canada are generally well tolerated and associated with minimal side effects.
If I Drink Alcohol And/or Use Recreational Drugs Is It Safe To Take Prep
Alcohol and recreational drugs are not known to interact with PrEP medications. It is safe to take PrEP before, after and on days when you are partying. In fact, it is important to take extra steps to make sure you take PrEP according to the healthcare providers directions when you are partying.
Don’t Miss: What Percent Of Gay People Have Hiv
The Recommended Pep Regimens Are:
- For adults: Tenofovir combined with either lamivudine or emtricitabine as preferred backbone drugs and these are also the preferred drugs for treating HIV. The recommended third drug is ritonavir-boosted lopinavir , which is also recommended by WHO as a preferred drug for HIV treatment
- For children: Zidovidune and lamivudine backbone drugs for children aged 10 or below, with ritonavir-boosted lopinavir recommended as the third drug choice. This is also in alignment with preferred drugs for treating HIV in children
Baseline Testing Of The Exposed Individual
Reviewed and updated: Medical Care Criteria Committee August 11, 2022
Lead authors for material on PEP in children: Aracelis Fernandez, MD, with Lisa-Gaye Robinson, MD, and Ruby Fayorsey, MD, with the Medical Care Criteria Committee June 2020
Baseline HIV testing of the exposed individual identifies individuals who were already infected with HIV at the time of presentation . Results may inform decision-making regarding initiation of ART as treatment for established infection or initiation of 28 days of PEP to prevent HIV infection .
An initial reactive screening result must be confirmed with an HIV Ab differentiation immunoassay, and the PEP regimen should be continued until that result is obtained. Furthermore, the PEP regimen should be continued as rapid ART initiation if the reactive result is confirmed with an Ab differentiation immunoassay or HIV-1 RNA test, and the exposed individual should be referred to an experienced HIV care provider.
| KEY POINTS |
|
Also Check: Is Hiv Contagious If On Medication