Hiv Education And Approach To Comprehensive Sexuality Education
Sex education in schools is widespread in Western Europe, with many countries in this area of the region taking a comprehensive approach by including topics such as sexuality, gender inequality and gender norms, alongside topics such as pregnancy, contraception and STIs including HIV.71 A similar situation exists across Canada.
In stark contrast, sexuality education in Central European countries tends to reduce it to a basic anatomical study of the human body and the promotion of abstinence, traditional family values marriage and religious morality.72
In the USA, only 13 states require sexulaity education to be medically accurate, creating disparities in what children learn. Even when sexulaity education is required, state policies vary widely, and a number of states leave issues such as sexuality, gender identity and contraception unaddressed. Many link this to the fact that, in 2016, the USA had higher rates of teen pregnancy and STIs among teenagers than most other high-income countries.73
Hiv And Sex Education
The status of sexual health education varies substantially throughout the USA and is insufficient in many areas. In most states, fewer than half of high schools teach all 16 topics CDC recommends for effective sex education. Many also argue that sex education is not starting early enough.71
The percentage of schools in which students are required to receive instruction on HIV prevention is decreasing, from 64% in 2000 to 41% in 2014.72
Conservative support for abstinence-only sex education has also been a major barrier to progress, and has been shown to be associated with increased HIV rates among adolescents.73
President Obama eliminated three-quarters of the budget for abstinence-only sex education in 2009, which had previously received the majority of funding.7475 However, funding for abstinence-only sex education began to rise again in the following years and stood at US $85 million in 2016.76
In February 2018, this was renewed for two more years at US $75 million annually under the new name of sexual risk avoidance education.77 As of 2019, 37 states require that information on abstinence be provided, 27 of which require for abstinence to be emphasised, with the 10 remaining states requiring that abstinence is covered. In contrast, only 12 states require discussion of sexual orientation. Of these, nine states require that discussion be inclusive.78
Hiv Prevalence By Region Of Residence
In the United States, based on data for persons with diagnosed or undiagnosed HIV at year-end 2019, more persons with HIV resided in the South than any other region . Overall, at year-end 2019, 46% of persons with diagnosed or undiagnosed HIV resided in the South, 22% in the Northeast, 20% in the West, and 12% in the Midwest . The HIV prevalence rate by region was highest in the Northeast and second highest in the South.
Also Check: Can You Get Aids From Dried Blood
The Epidemiology Of Hiv In Canada
This fact sheet provides a snapshot of the HIV epidemic in Canada. All epidemiological information is approximate, based on the best available data. Most of the data contained in this fact sheet come from the latest estimates from the Public Health Agency of Canada, which are for the year 2018. More information can be found in the section Where do these numbers come from? at the end of the fact sheet.
In 2019 36060 People Lived With Hiv In Atlanta As Per Atlanta Hiv Rates
Moreover, Atlanta had 1,530 new cases in 2018. According to the data on the Atlanta HIV rate, 80% of the cases were males, and more than 70% of those affected were Black. Then, nearly 71% of the male transmissions stemmed from male-to-male sexual contact. And stats on HIV transmission rates found that almost 60% of the female transmissions occurred due to heterosexual contact.
You May Like: Hiv From Dried Blood
Hiv And Tuberculosis In India
India is one of the WHOs 30 high TB burden countries. Globally, 10 million people are estimated to have developed tuberculosis in 2017, 27% of whom lived in India.90
Multi drug-resistant TB continues to be a public health issue. Of the three countries accounting for almost half of the worlds MDR/RR-TB cases in 2017, India has the highest proportion at 24%, followed by China at 13% and Russia at 10%.91
In 2017, 11% of people newly enrolled in HIV care in India had active TB. Of the 410,000 people who died of TB in 2017, 11,000 were HIV positive.92In 2017, 58% of people with HIV-associated TB were not reported to have reached TB care. Reasons for missing people with TB include poor integration of and lack of access to services, weaknesses in service delivery, gaps in recording and reporting, and limited private sector engagement.93
To strengthen integration, the government has been rolling out TB service delivery from all HIV clinics since December 2016.94 Although reporting of HIV case-based data for the TB case-finding cascade has not yet been possible, NACO has been able to report data based on clinic visits. People living with HIV made almost 11 million visits to ART centres in 2017. In 83% of these visits, clinic attendees received an evaluation for TB. Of those who were evaluated, 6% had TB symptoms.95 Coverage of treatment to prevent TB among people living with HIV is low, with only 42% of those eligible for Isoniazid Preventive Therapy receiving it as of 2019.96
Is Canada Reaching The Global 90
The Joint United Nations Programme on HIV/AIDS and the World Health Organization have established a global health sector strategy on HIV to help eliminate AIDS as a public health threat by 2030. Canada has endorsed this strategy. The strategy can be encapsulated in the phrase 90-90-90 and consists of the following targets for the year 2020:
- 90% of people with HIV know their infection status
- 90% of people diagnosed with HIV receive HIV treatment
- 90% of people taking treatment have an undetectable viral load
Canada is approaching the 90% goal for awareness of HIV status and the 90% goal for treatment and has surpassed the 90% goal for achieving viral suppression. Of the estimated 62,050 people with HIV in Canada in 2018, an estimated:
- 87% were diagnosed and aware they had HIV
- 85% of those who were diagnosed were on treatment
- 94% of those on treatment had achieved viral suppression
This means that 70% of all Canadians with HIV had achieved viral suppression in 2018. If all 90-90-90 measures had been reached, 73% of all Canadians with HIV would have achieved viral suppression.
Recommended Reading: How Long Does It Take For Hiv To Become Aids
Deaths Of Persons Diagnosed With Hiv Or Aids
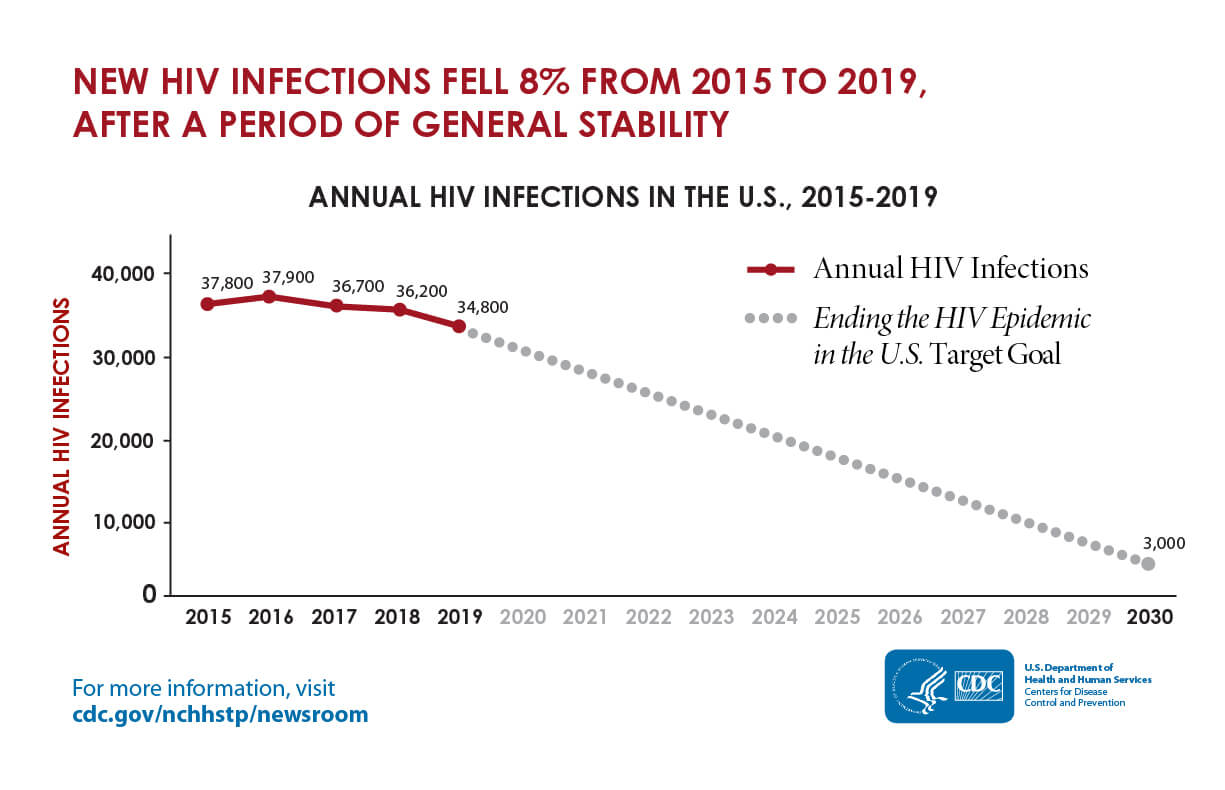
With the availability of potent combination antiretroviral therapy in the mid-1990s, the annual number of HIV-related deaths in the United States dramatically decreased. Subsequently, from 2000 to 2011 the number of annual deaths of persons ever diagnosed with AIDS continued to decline. More recently, CDC surveillance data revealed that during 2015 to 2019 the annual number of deaths of persons diagnosed with HIV has remained stable at approximately 16,000 deaths per year . Note, however, that deaths of persons with HIV , as reported, may be due to any cause and may be unrelated to HIV or AIDS. Recent analysis suggests that persons with HIV infection who take antiretroviral therapy have a life expectancy of 71 years.
Estimates Number Of New Hiv Infections
The Agency estimates that 2,242 new infections occurred in Canada in 2018. This estimate is a slight increase from the estimate for 2016 .
The resulting estimated incidence rate in Canada for 2018 was 6.0 per 100,000 population which is a slight increase from the estimate for 2016 .
Figure 8. HIV incidence: Estimated annual number of new HIV infections in Canada
This graph shows the point estimates of new HIV infections by year with each associated plausible ranges for point estimates. The vertical axis shows the estimated number of new HIV infections per year, with the low and high ranges. The horizontal axis shows the calendar years.
| Year |
|---|
| gbMSM-PWID | 2.7% |
Among the estimated new infections in 2018, an estimated 1,109 were among gay, bisexual and other men who have sex with men , representing just under half of all new HIV infections in 2018, despite representing approximately 3-4% of the Canadian adult male population. Although the gbMSM population continues to be over-represented in new HIV infections in Canada, the proportion of new infections among this population has decreased compared to 2016. .
Three hundred and twelve of the estimated new infections in 2018 were among people who inject drugs , accounting for 13.9% of new infections. The proportion of new infections attributed to heterosexuals increased slightly to 34.0% from 31.7% in 2016.
Read Also: Is Hair Loss A Symptom Of Hiv
Hiv Statistics By State
Human immunodeficiency virus, or HIV, is a virus that weakens a persons immune system by attacking cells that fight off infection, specifically a persons CD4 cells. HIV is spread through body fluids such as blood. If HIV goes untreated and advances, it can lead to acquired immunodeficiency syndrome or AIDS.
Unlike most other viruses, when a person contracts HIV, they have it for life because the human body cannot fight off the virus entirely. HIV, however, can be controlled and its progression can be slowed significantly. There are three stages of HIV:
Hiv Education And Approach To Sex Education
Increasing awareness among the general population and key affected populations about HIV prevention is a central focus of NACP IV. However, as of 2017, only 22% of young women and 32% of young men knew how to prevent HIV.53 This is reflected in the wider population, as only one-fifth of women and one-third of men had comprehensive knowledge of HIV and AIDS.54
A number of innovative awareness programmes are being implemented. In 2018, NACO ran a multimedia HIV campaign to increase HIV testing among young people. This ran on Doordarshan, cable and satellite channels, radio, online and at cinemas. NACO also broadcasts phone-in and panel discussions on issues relating to HIV on regional radio networks. Shows relating to HIV are also performed by folk troupes in remote villages to reach people in places with no television or radio.55
Through Indias Adolescent Education Programme, comprehensive sexuality education is available in schools for students aged between 13 and 18.56The AEP was operating in 55,000 schools as of 2018/19.57
Indias CSE curriculum covers a wide range of issues relating to sexual and reproductive health . However, it excludes sexual rights and diverse sexual orientations, gender identities, and negotiation and decision-making skills within sexual relationships.58
You May Like: Hiv Without Ejaculation
New Hiv Diagnosis By Race/ethnicity
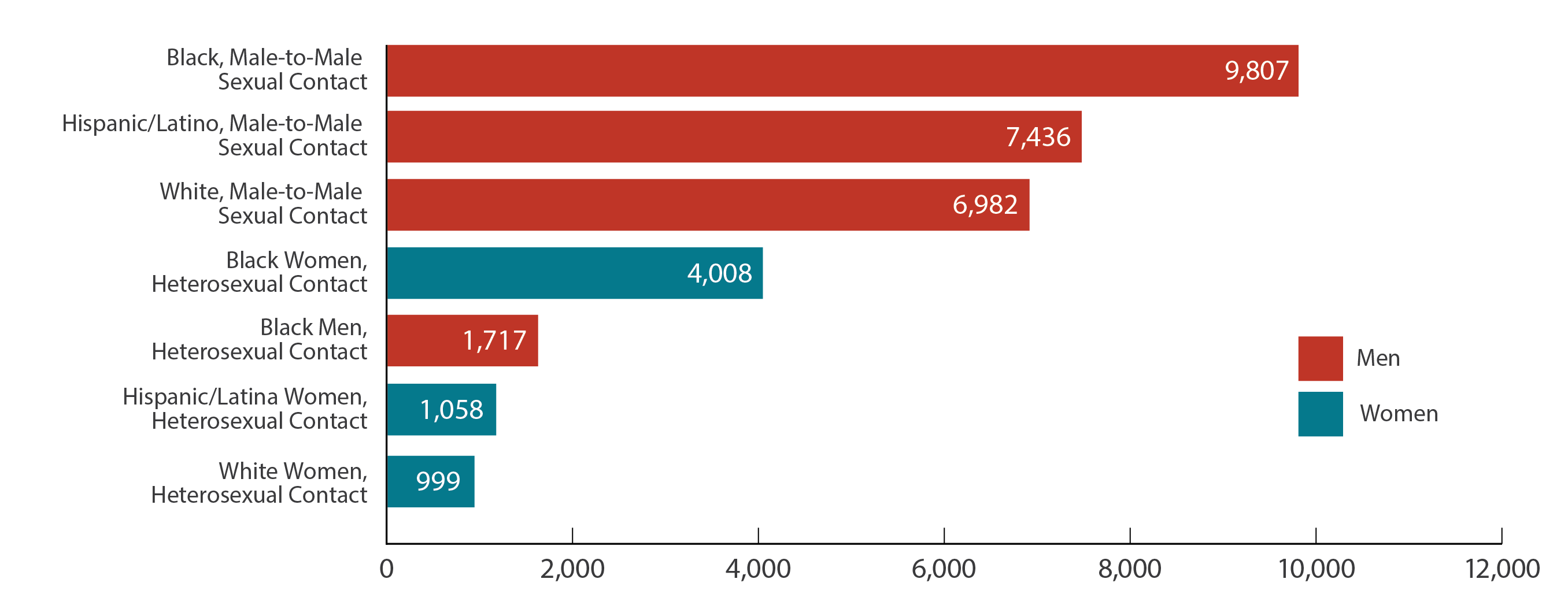
Of the persons diagnosed with HIV in 2019 in the United States, 42.1% were among persons who are Black/African American, 27.8% Hispanic/Latino, 24.8% White, 2% Asian, 2.5% persons of multiracial, and less than 1% each for persons who are American Indian/Alaska Native and Native Hawaiian/other Pacific Islander. The number and rate of new HIV diagnoses in 2019 was highest in persons who are Black/African American. The rate of new diagnosis in 2019 among Black/African American persons approximately 8.1 times higher than persons who are White .
Strutural And Resource Barriers
In recent years, there have been shortfalls in the procurement, management and distribution of ARVs, HIV testing kits and other HIV commodities, mainly due to supply chain bottlenecks.108
India is large and the status of infrastructure varies widely across the country The operation of the system, particularly in remote locations, needs to be strengthened. For example, slow internet speeds can really disrupt the system. Late payments to drug companies has also led to delays in the delivery of medicines.
– Ashok Kumar Agarwal at Public Health Foundation of India109
Don’t Miss: Is Hiv In Semen
Is The World Making Progress In Its Fight Against Hiv/aids
The 1990s saw a substantial increase in the number of people infected with HIV and dying of AIDS.
Between 1996 and 2001 more than 3 million people were infected with HIV ever year. Since then the number of new infections began to decline and in 2017 it was reduced to below 2 million. The lowest number of new infections since 1990.
The number of AIDS-related deaths increased throughout the 1990s and reached a peak in 2005, 2006 when in both years close to 2 million people died. Since then the annual number of deaths from AIDS declined as well and was since halved. 2017 was the first year since the peak in which fewer than 1 million people died from AIDS.
The chart also shows the continuing increase in the number of people living with HIV. The rate of increase has slowed down compared to the 1990s, but the absolute number is at the highest ever with more than 36 million people globally living with HIV.
What Is The Mortality Rate Of Hiv Infection
Mortality from HIV disease has not been among the 15 leading causes of death in the US since 1997. The age-adjusted death rate for HIV disease peaked in 1995 at 16.3 per 100,000 population, decreased 69.9% through 1998, then further decreased 30.2% from 1999 through 2007, to 3.7 per 100,000 population. In 2007, a total of 11,295 persons died from HIV disease. However, HIV disease has remained among the 5 leading causes of death for specific age groups for females, and in the black population.
Don’t Miss: How Long Can Aids Go Undetected
Hiv Testing And Counselling In Western And Central Europe And North America
The number of HIV tests performed in Western and Central Europe and the USA continues to steadily increase. By 2016, two European countriesDenmark and Swedenhad already met the UNAIDS target of diagnosing 90% of people living with HIV, and another 10 European countries plus the USA reported that 85% or more people living with HIV were aware of their status.54
In 2016, only three countries in Western and Central Europe – France, Norway and the UK – had laws and policies in place authorising self-testing. Saliva-based self-testing kits have been available in the USA since 2012.55
Late diagnoses of HIV, indicated by low CD4 counts, remain a major issue. Nearly a quarter of all people in Western and Central Europe diagnosed with HIV between 2014 and 2016 recorded CD4 T-cell counts below 200 cells/mm³.56
In 2016, more than half of people diagnosed with HIV were diagnosed with CD4 counts under 350 in eight countries Western and Central Europe: 66% in Lithuania, 64% in Romania , 58% in Greece, 56% in Croatia, 56% in Italy, 54% in Estonia, 52% in Finland and 51% in Germany.57
In Canada, 25% of people living with HIV are unaware of their status.61 Less than 50% of men who have sex with men have tested for HIV. However, testing rates among people who inject drugs is high at more than 75%.62
Cities With The Highest Hiv Rates
Around 1.1 million people are living with HIV in the United States of America . Nearly one in seven of these people are unaware they have HIV.
The size of the HIV epidemic is relatively small compared to the countrys population, but is heavily concentrated among several key affected populations. Around 70% of annual new HIV infections occur among gay and other men who have sex with men , among whom African American/black men are most affected, followed by Latino/Hispanic men.
Heterosexual African American/black women and transgender women of all ethnicities are also disproportionately affected.
The USA is the greatest funder of the global response to HIV, but also has an ongoing HIV epidemic itself, with around 37,600 new infections a year. HIV affects locations differently as well, so weve compiled the cities with highest rates in the nation .
You May Also Like
10. Baltimore, Maryland 24.3
According to GetTested.com, HIV infection rates in Baltimore are on the rise due to a lack of education. HIV is a lifelong infection that, if left untreated, can lead to AIDS , according to HIV.gov.
AIDS occurs when a persons immune system becomes damaged, and people who are diagnosed with AIDS typically survive about three years.
9. Jacksonville, Florida 25.1
Although Jacksonville isnt thought of as a party city like other destinations on GetTested.coms list, the site suggests that
Also Check: How Long Can Hiv Be Dormant In Your System
Tuberculosis Among People Living With Hiv
Tuberculosis is the leading HIV-associated opportunistic infection in low- and middle- income countries, and it is a leading cause of death globally among people living with HIV. Death due to tuberculosis still remains high among people living with HIV, however the number of deaths is decreasing. Most of the global mortality due to TB among those with HIV is from cases in Sub-Saharan Africa.
In the charts here we see the number of tuberculosis patients who tested positive for HIV the number receiving antiretroviral therapy and the number of TB-related deaths among those living with HIV.
People who use ART are living longer
ART not only saves lives but also gives a chance for people living with HIV/AIDS to live long lives. Without ART very few infected people survive beyond ten years.3
Today, a person living in a high-income country who started ART in their twenties can expect to live for another 46 years that is well into their 60s.4
While the life expectancy of people living with HIV/AIDS in high-income countries has still not reached the life expectancy of the general population, we are getting closer to this goal.5
ART prevents new HIV infections
There is considerable evidence to show that people who use ART are less likely to transmit HIV to another person.7 ART reduces the number of viral particles present in an HIV-positive individual and therefore, the likelihood of passing the virus to another person decreases.
We need to increase ART coverage